
Philip Scheltens (born 1957) is a Dutch professor of neurology and founder of the Alzheimer Centre, Amsterdam University Medical Centers, location VUmc in Amsterdam.

Philip Scheltens (born 1957) is a Dutch professor of neurology and founder of the Alzheimer Centre, Amsterdam University Medical Centers, location VUmc in Amsterdam.
Philip Scheltens was born in Dordrecht, Netherlands, where he grew up in a family of four. His father led a factory. His grandfather developed Alzheimer's disease in those years, which made an impression on his grandson. Philip attended the Christelijk Lyceum, where he graduated in 1976. As a teenager he was an enthusiastic drummer in several bands and was fascinated by science and mechanics.
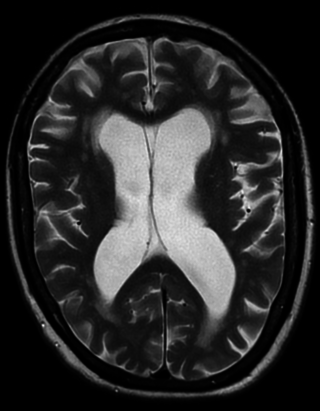
After his graduation, he studied medicine at the Vrije Universiteit (VU) Amsterdam. He obtained his medical degree in 1984 and started his career in neurology. During his PhD, which he defended and received om March 3, 1993, he developed MRI criteria to score hippocampus atrophy for the diagnosis of Alzheimer's disease. In 2000 he was appointed professor of Cognitive Neurology at the Vrije Universiteit Amsterdam. In that same year he founded the Alzheimer Center, which he directed until end of 2021. As from 2022 he is staff neurologist at the Alzheimer Center which he combines with his role as head of EQT Life Sciences Dementia Fund (formerly known as LSP).
Scheltens' work has changed the way Alzheimer's disease is diagnosed. While diagnosis used to be based on specific signs and symptoms and exclusion of treatable causes, he was the first to add MRI criteria for hippocampal atrophy, associated with Alzheimer's' disease in the 1990s, which improved the diagnostic classification of this type of dementia and fueled development of new diagnostics.
He was one of the first in the Netherlands to start a dementia clinic and started the Amsterdam Dementia cohort, currently the largest collection of clinical and biomarker data. This enabled him to initiate, together with colleagues, new diagnostic research criteria for Alzheimer's disease based on the presence of a clinical phenotype and the presence of amyloid, as reflected in cerebrospinal fluid. This change from a phenomenological, purely symptom driven, diagnosis to a diagnosis based on biomarkers greatly enhanced sensitivity and specificity. Higher diagnostic precision is the crucial step to develop effective therapy, as patients with homogeneous underlying pathology can be included for therapeutic trials targeting the causative mechanism. The new protein-based diagnostic criteria he fathered are now implemented for trials worldwide and the first hopeful results have emerged.
Scheltens has improved societal awareness and acceptance of dementia, and prioritized dementia among the top necessities on the Dutch and European research agenda. He initiated a large scientific and societal action plan to improve prevention, treatment and care for dementia in the Netherlands, entitled Deltaplan Dementie in 2012, which has already supported a large number of research projects on dementia, increased societal awareness and improved health care for dementia patients.
In 2011 Scheltens became a member of the Royal Netherlands Academy of Arts and Sciences (KNAW). [1]
In November 2018 Expertscape recognized Dr. Scheltens as #6 in the world for expertise in Alzheimer's disease. [2]
Scheltens has authored or coauthored over 1100 publications [4]

Dementia with Lewy bodies (DLB) is a type of dementia characterized by changes in sleep, behavior, cognition, movement, and regulation of automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive impairment interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the prevalence is not known accurately and many diagnoses are missed. The disease was first described on autopsy by Kenji Kosaka in 1976, and he named the condition several years later.
Vascular dementia is dementia caused by a series of strokes. Restricted blood flow due to strokes reduces oxygen and glucose delivery to the brain, causing cell injury and neurological deficits in the affected region. Subtypes of vascular dementia include subcortical vascular dementia, multi-infarct dementia, stroke-related dementia, and mixed dementia.

Binswanger's disease, also known as subcortical leukoencephalopathy and subcortical arteriosclerotic encephalopathy, is a form of small-vessel vascular dementia caused by damage to the white brain matter. White matter atrophy can be caused by many circumstances including chronic hypertension as well as old age. This disease is characterized by loss of memory and intellectual function and by changes in mood. These changes encompass what are known as executive functions of the brain. It usually presents between 54 and 66 years of age, and the first symptoms are usually mental deterioration or stroke.

Frontotemporal dementia (FTD), frontotemporal degeneration disease, or frontotemporal neurocognitive disorder encompasses several types of dementia involving the progressive degeneration of the brain's frontal and temporal lobes. FTDs broadly present as behavioral or language disorders with gradual onsets.
Parkinson-plus syndromes (PPS) are a group of neurodegenerative diseases featuring the classical features of Parkinson's disease with additional features that distinguish them from simple idiopathic Parkinson's disease (PD). Parkinson-plus syndromes are either inherited genetically or occur sporadically.

Corticobasal degeneration (CBD) is a rare neurodegenerative disease involving the cerebral cortex and the basal ganglia. CBD symptoms typically begin in people from 50 to 70 years of age, and typical survival before death is eight years. It is characterized by marked disorders in movement and cognition, and is classified as one of the Parkinson plus syndromes. Diagnosis is difficult, as symptoms are often similar to those of other disorders, such as Parkinson's disease, progressive supranuclear palsy, and dementia with Lewy bodies, and a definitive diagnosis of CBD can only be made upon neuropathologic examination.
Psychoorganic syndrome (POS), also known as organic psychosyndrome, is a progressive disease comparable to presenile dementia. It consists of psychopathological complex of symptoms that are caused by organic brain disorders that involve a reduction in memory and intellect. Psychoorganic syndrome is often accompanied by asthenia.
Alcohol-related dementia (ARD) is a form of dementia caused by long-term, excessive consumption of alcohol, resulting in neurological damage and impaired cognitive function.
Mild cognitive impairment (MCI) is a neurocognitive disorder which involves cognitive impairments beyond those expected based on an individual's age and education but which are not significant enough to interfere with instrumental activities of daily living. MCI may occur as a transitional stage between normal aging and dementia, especially Alzheimer's disease. It includes both memory and non-memory impairments. The cause of the disorder remains unclear, as well as both its prevention and treatment, with some 50 percent of people diagnosed with it going on to develop Alzheimer's disease within five years. The diagnosis can also serve as an early indicator for other types of dementia, although MCI may remain stable or even remit.
The NINCDS-ADRDA Alzheimer's Criteria were proposed in 1984 by the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association and are among the most used in the diagnosis of Alzheimer's disease (AD). These criteria require that the presence of cognitive impairment and a suspected dementia syndrome be confirmed by neuropsychological testing for a clinical diagnosis of possible or probable AD; while they need histopathologic confirmation for the definitive diagnosis. They specify as well eight cognitive domains that may be impaired in AD. These criteria have shown good reliability and validity.

Posterior cortical atrophy (PCA), also called Benson's syndrome, is a rare form of dementia which is considered a visual variant or an atypical variant of Alzheimer's disease (AD). The disease causes atrophy of the posterior part of the cerebral cortex, resulting in the progressive disruption of complex visual processing. PCA was first described by D. Frank Benson in 1988.

Alzheimer's disease (AD) is a neurodegenerative disease that usually starts slowly and progressively worsens, and is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in remembering recent events. As the disease advances, symptoms can include problems with language, disorientation, mood swings, loss of motivation, self-neglect, and behavioral issues. As a person's condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the average life expectancy following diagnosis is three to twelve years.
Samuel E. Gandy, is a neurologist, cell biologist, Alzheimer's disease (AD) researcher and expert in the metabolism of the sticky substance called amyloid that clogs the brain in patients with Alzheimer's. His team discovered the first drugs that could lower the formation of amyloid.
Gregor Karl Wenning was a German neurologist best known for his clinical and scientific work in Parkinson's disease and atypical Parkinsonian disorders, particularly multiple system atrophy (MSA). In 2006 he was appointed Professor and Head of the Division of Clinical Neurobiology at the Medical University Innsbruck. Wenning died on 11 February 2024, at the age of 59.
Clinical neuroscience is a branch of neuroscience that focuses on the scientific study of fundamental mechanisms that underlie diseases and disorders of the brain and central nervous system. It seeks to develop new ways of conceptualizing and diagnosing such disorders and ultimately of developing novel treatments.

neuGRID is a web portal aimed to (i) help neuroscientists do high-throughput imaging research, and (ii) provide clinical neurologists automated diagnostic imaging markers of neurodegenerative diseases for individual patient diagnosis. neuGRID's user-friendly environment is customised to a range of users from students to senior neuroscientists working in the fields of Alzheimer's disease, psychiatric diseases, and white matter diseases. neuGRID aims to become a widespread resource for brain imaging analyses.
Florbetaben, a fluorine-18 (18F)-labeled stilbene derivative, trade name NeuraCeq, is a diagnostic radiotracer developed for routine clinical application to visualize β-amyloid plaques in the brain. It is indicated for Positron Emission Tomography (PET) imaging of β-amyloid neuritic plaque density in the brains of adult patients with cognitive impairment who are being evaluated for Alzheimer's disease (AD) and other causes of cognitive impairment. β-amyloid is a key neuropathological hallmark of AD, so markers of β-amyloid plaque accumulation in the brain are useful in distinguishing AD from other causes of dementia. The tracer successfully completed a global multicenter phase 0–III development program and obtained approval in Europe, US and South Korea in 2014.
The Dementia with Lewy Bodies Consortium is an international multidisciplinary collaboration of researchers interested in the dementia with Lewy bodies. It first convened in Newcastle upon Tyne, England, in October 1995. Between 1995 and 2005, it issued three DLBC Consensus Reports on dementia with Lewy bodies.
Corticobasal syndrome (CBS) is a rare, progressive atypical Parkinsonism syndrome and is a tauopathy related to frontotemporal dementia. CBS is typically caused by the deposit of tau proteins forming in different areas of the brain.
Frederik Barkhof is a neuroradiologist. He led the development of the Barkhof Criteria for using MRI findings to predict conversion to clinically definite multiple sclerosis.