Related Research Articles

The endometrium is the inner epithelial layer, along with its mucous membrane, of the mammalian uterus. It has a basal layer and a functional layer: the basal layer contains stem cells which regenerate the functional layer. The functional layer thickens and then is shed during menstruation in humans and some other mammals, including apes, Old World monkeys, some species of bat, the elephant shrew and the Cairo spiny mouse. In most other mammals, the endometrium is reabsorbed in the estrous cycle. During pregnancy, the glands and blood vessels in the endometrium further increase in size and number. Vascular spaces fuse and become interconnected, forming the placenta, which supplies oxygen and nutrition to the embryo and fetus. The speculated presence of an endometrial microbiota has been argued against.

In mammals, pregnancy is the period of reproduction during which a female carries one or more live offspring from implantation in the uterus through gestation. It begins when a fertilized zygote implants in the female's uterus, and ends once it leaves the uterus.

The uterus or womb is the main hormone-responsive, secondary sex organ of the female reproductive system in humans, and most other mammals. Events occurring within the uterus are described with the term in utero. In the human, the lower end of the uterus, the cervix, opens into the vagina, while the upper end, the fundus, is connected to the fallopian tubes. It is within the uterus that the embryo and later fetus develops during gestation. In the human embryo, the uterus develops from the paramesonephric ducts which fuse into the single organ known as a simplex uterus. The uterus has different forms in many other animals and in some it exists as two separate uteri known as a duplex uterus.

The blastocyst is a structure formed in the early development of mammals. It possesses an inner cell mass (ICM) which subsequently forms the embryo. The outer layer of the blastocyst consists of cells collectively called the trophoblast. This layer surrounds the inner cell mass and a fluid-filled cavity known as the blastocoel. The trophoblast gives rise to the chorion and amnion that surround the embryo. The placenta derives from the embryonic chorion and the underlying uterine tissue of the mother. The name "blastocyst" arises from the Greek βλαστός blastos and κύστις kystis. In other animals this is a structure consisting of an undifferentiated ball of cells and is called a blastula.
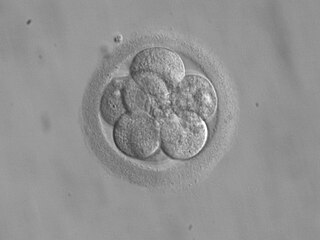
Embryo transfer refers to a step in the process of assisted reproduction in which embryos are placed into the uterus of a female with the intent to establish a pregnancy. This technique (which is often used in connection with in vitro fertilization, may be used in humans or in animals, in which situations the goals may vary.

Adenomyosis is a medical condition characterized by the growth of cells that proliferate on the inside of the uterus (endometrium) atypically located among the cells of the uterine wall (myometrium), as a result, thickening of the uterus occurs. As well as being misplaced in patients with this condition, endometrial tissue is completely functional. The tissue thickens, sheds and bleeds during every menstrual cycle.

Endometritis is inflammation of the inner lining of the uterus (endometrium). Symptoms may include fever, lower abdominal pain, and abnormal vaginal bleeding or discharge. It is the most common cause of infection after childbirth. It is also part of spectrum of diseases that make up pelvic inflammatory disease.

"Cytotrophoblast" is the name given to both the inner layer of the trophoblast or the cells that live there. It is interior to the syncytiotrophoblast and external to the wall of the blastocyst in a developing embryo.
Autologous Endometrial Coculture is a technique of assisted reproductive technology. It involves placing a patient’s fertilized eggs on top of a layer of cells from her own uterine lining, creating a more natural environment for embryo development and maximizing the chance for an in vitro fertilization (IVF) pregnancy.

In female mammals implantation is the stage in embryonic development in which the blastocyst hatches as the embryo, and adheres to the wall of the uterus. Once this adhesion is successful, the female is considered to be pregnant and the embryo will receive oxygen and nutrients from the mother in order to grow.

Decidualization is a process that results in significant changes to cells of the endometrium in preparation for, and during, pregnancy. This includes morphological and functional changes to endometrial stromal cells (ESCs), the presence of decidual white blood cells (leukocytes), and vascular changes to maternal arteries. The sum of these changes results in the endometrium changing into a structure called the decidua. In humans, the decidua is shed during childbirth.

Glycodelin(GD) also known as human placental protein-14 (PP-14)progestogen-associated endometrial protein (PAEP) or pregnancy-associated endometrial alpha-2 globulin is a glycoprotein that inhibits cell immune function and plays an essential role in the pregnancy process. In humans is encoded by the PAEP gene.

VEZT is a gene located on chromosome 12 and encodes for the protein vezatin. Vezatin is a major component of the cadherin-catenin complex that is critical to the formation and maintenance of adherens junctions. The protein is expressed in most epithelial cells and is crucial to the formation of cell-cell contact junctions. Mutations of the gene can lead to upregulation or downregulation of the protein which can have detrimental effects on physiological systems, particularly those involved in development.
Pinopodes are protrusions on the apical cellular membrane of uterine epithelial cells.
Hormonal regulation occurs at every stage of development. A milieu of hormones simultaneously affects development of the fetus during embryogenesis and the mother, including human chorionic gonadotropin (hCG) and progesterone (P4).
Menstruation is the shedding of the uterine lining (endometrium). It occurs on a regular basis in uninseminated sexually reproductive-age females of certain mammal species.
The internal surface of the uterus is lined by uterine epithelial cells which undergo dramatic changes during pregnancy. The role of the uterine epithelial cells is to selectively allow the blastocyst to implant at a specific time. All other times of the cycle, these uterine epithelial cells are refractory to blastocyst implantation. Uterine epithelial cells have a similar structure in most species and the changes which occur in the uterine epithelial cells at the time of blastocyst implantation are also conserved among most species.

A t-shaped uterus is a type of uterine malformation wherein the uterus is shaped resembling the letter T. This is typically observed in DES-exposed women. It is recognised in the ESHRE/ESGE classification, and is associated with failed implantation, increased risk of ectopic pregnancy, miscarriage and preterm delivery. There is a surgical procedure to correct the malformation.

The uterine microbiome is the commensal, nonpathogenic, bacteria, viruses, yeasts/fungi present in a healthy uterus, amniotic fluid and endometrium and the specific environment which they inhabit. It has been only recently confirmed that the uterus and its tissues are not sterile. Due to improved 16S rRNA gene sequencing techniques, detection of bacteria that are present in low numbers is possible. Using this procedure that allows the detection of bacteria that cannot be cultured outside the body, studies of microbiota present in the uterus are expected to increase.
Repeated Implantation failure (RIF) is the failure of the embryo to implant onto the side of the uterus wall following IVF treatment. Regularly, this happens at 6–7 days after conception and involves the embedding of the growing embryo into the mothers uterus and a connection being formed. A successful implantation can be determined by using an ultrasound to view the sac which the baby grows in, inside the uterus.
References
- ↑ Murphy, C.R. The plasma membrane of uterine epithelial cells: structure and histochemistry. Gustav Fischer Verlag: Stuttgart and New York. 1993. ( ISBN 3-437-11514-6). (also published as Progress in Histochemistry and Cytochemistry, volume 27, no. 3).
- ↑ Murphy, C.R. and T.J. Shaw. Plasma membrane transformation: a common response of uterine epithelial cells during the peri-implantation period. Cell Biology International 18: 1115-1128. 1994.
- ↑ Garrido-Gomez et al. Profiling the gene signature of endometrial receptivity: clinical results. Fertility and Sterility: 99: 1079-1085. 2013.
- ↑ Gipson, Ilene K., et al. "MUC16 is lost from the uterodome (pinopode) surface of the receptive human endometrium: in vitro evidence that MUC16 is a barrier to trophoblast adherence." Biology of reproduction 78.1 (2008): 134-142.
- ↑ Kabir-Salmani, M., Nikzad, H., Shiokawa, S., Akimoto, Y., & Iwashita, M. (2005). Secretory role for human uterodomes (pinopods): secretion of LIF. Molecular human reproduction, 11(8), 553-559.
- ↑ Kurihara, I., Lee, D. K., Petit, F. G., Jeong, J., Lee, K., Lydon, J. P., ... & Tsai, S. Y. (2007). COUP-TFII mediates progesterone regulation of uterine implantation by controlling ER activity. PLoS Genetics, 3(6), e102. doi:10.1371/journal.pgen.0030102
- ↑ Díaz-Gimeno, P., Horcajadas, J. A., Martínez-Conejero, J. A., Esteban, F. J., Alamá, P., Pellicer, A., & Simón, C. (2011). A genomic diagnostic tool for human endometrial receptivity based on the transcriptomic signature. Fertility and sterility, 95(1), 50-60.
- ↑ Chen, Jenny IC, Natalie J. Hannan, Yunxian Mak, Peter K. Nicholls, Jin Zhang, Adam Rainczuk, Peter G. Stanton, David M. Robertson, Lois A. Salamonsen, and Andrew N. Stephens. "Proteomic characterization of midproliferative and midsecretory human endometrium." Journal of Proteome Research 8, no. 4 (2009): 2032-2044.
- ↑ Murphy, C.R. Junctional barrier complexes undergo major alterations during the plasma membrane transformation of uterine epithelial cells. Human Reproduction 15, Supplement 3: 182-188. 2000.
- ↑ Murphy, C.R., M.J. Hosie and M.B. Thompson. The plasma membrane transformation facilitates pregnancy in both reptiles and lizards. Comparative Biochemistry and Physiology A 127: 433-439. 2000.
- ↑ Murphy, C.R. Uterine receptivity and the plasma membrane transformation. Cell Research 14: 258-267. 2004.