Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that can develop because of exposure to a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event. Young children are less likely to show distress but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.
Psychological trauma, mental trauma or psychotrauma is an emotional response to a distressing event or series of events, such as accidents, rape, or natural disasters. Reactions such as psychological shock and psychological denial are typical. Longer-term reactions include unpredictable emotions, flashbacks, difficulties with interpersonal relationships and sometimes physical symptoms including headaches or nausea.

Wounded in Action (WIA) describes combatants who have been wounded while fighting in a combat zone during wartime, but have not been killed. Typically, it implies that they are temporarily or permanently incapable of bearing arms or continuing to fight. Generally, the Wounded in Action are far more numerous than those killed. Common combat injuries include second and third degree burns, broken bones, shrapnel wounds, brain injuries, spinal cord injuries, nerve damage, paralysis, loss of sight and hearing, post-traumatic stress disorder (PTSD), and limb loss.
Adjustment disorder is a maladaptive response to a psychosocial stressor. It is classified as a mental disorder. The maladaptive response usually involves otherwise normal emotional and behavioral reactions that manifest more intensely than usual, causing marked distress, preoccupation with the stressor and its consequences, and functional impairment.

Combat stress reaction (CSR) is acute behavioral disorganization as a direct result of the trauma of war. Also known as "combat fatigue", "battle fatigue", or "battle neurosis", it has some overlap with the diagnosis of acute stress reaction used in civilian psychiatry. It is historically linked to shell shock and can sometimes precurse post-traumatic stress disorder.

Operation Bayonet Lightning was a military operation during the early stages of the Iraq War, that was held to capture weapons, materials, and people who posed a threat against coalition forces. The joint operation between Iraq and the United States, lasted approximately 16 hours, and was conducted on 2 December 2003. 1,200 soldiers from the 173rd Airborne Brigade, the 4th Infantry Division, and Iraqi military participated. Operation Bayonet Lightning was concentrated on Al Hawija, Iraq, and the village of Rashad, Iraq, sixty kilometers, or thirty-seven miles, to the south of Kirkuk, Iraq.
Acute stress disorder is a psychological response to a terrifying, traumatic or surprising experience. It may bring about delayed stress reactions if not correctly addressed.
Complex post-traumatic stress disorder is a psychological disorder that is theorized to develop in response to exposure to a series of traumatic events in a context in which the individual perceives little or no chance of escape, and particularly where the exposure is prolonged or repetitive. It is not yet recognized by the American Psychiatric Association or the DSM-5 as a valid disorder, although was added to the eleventh revision of the International Classification of Diseases (ICD-11). In addition to the symptoms of post-traumatic stress disorder (PTSD), an individual with C-PTSD experiences emotional dysregulation, negative self-beliefs and feelings of shame, guilt or failure regarding the trauma, and interpersonal difficulties. C-PTSD relates to the trauma model of mental disorders and is associated with chronic sexual, psychological, and physical abuse or neglect, or chronic intimate partner violence, bullying, victims of kidnapping and hostage situations, indentured servants, victims of slavery and human trafficking, sweatshop workers, prisoners of war, concentration camp survivors, and prisoners kept in solitary confinement for a long period of time, or defectors from authoritarian religions. Situations involving captivity/entrapment can lead to C-PTSD-like symptoms, which can include prolonged feelings of terror, worthlessness, helplessness, and deformation of one's identity and sense of self. C-PTSD is linked to adverse childhood experiences, especially among survivors of foster care.
Peer support occurs when people provide knowledge, experience, emotional, social or practical help to each other. It commonly refers to an initiative consisting of trained supporters, and can take a number of forms such as peer mentoring, reflective listening, or counseling. Peer support is also used to refer to initiatives where colleagues, members of self-help organizations and others meet, in person or online, as equals to give each other connection and support on a reciprocal basis.
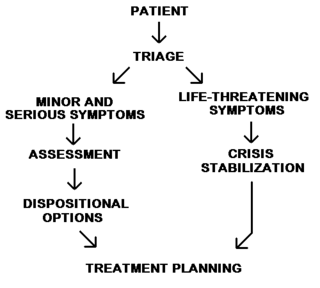
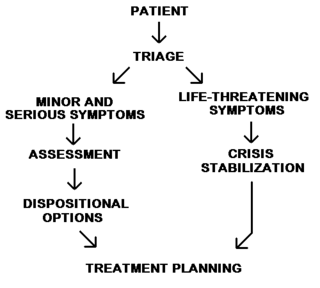
Psychiatric and mental health nurses in the U.S. Army Nurse Corps employing groundbreaking protocols and treatments in psychiatric issues to address the unique challenges that our service men and women face, more commonly post-traumatic stress disorder and traumatic brain injuries. Most people understand that trauma exposure is a popular occupational hazard for military members. Psychiatric screenings, before and during their enlistment, and treatments after being exposed to warfare, death, destruction, and torture have been extremely beneficial for military personnel and their dependents.
Exposure therapy is a technique in behavior therapy to treat anxiety disorders. Exposure therapy involves exposing the target patient to the anxiety source or its context without the intention to cause any danger (desensitization). Doing so is thought to help them overcome their anxiety or distress. Procedurally, it is similar to the fear extinction paradigm developed for studying laboratory rodents. Numerous studies have demonstrated its effectiveness in the treatment of disorders such as generalized anxiety disorder, social anxiety disorder, obsessive-compulsive disorder, post-traumatic stress disorder (PTSD), and specific phobias.
The ring leader of a cell responsible for conducting improvised explosive device attacks on the people and security forces of North Babil was captured by paratroopers south of Mahmudiyah, 11 July 2007.
Traumatic stress is a common term for reactive anxiety and depression, although it is not a medical term and is not included in the Diagnostic and Statistical Manual of Mental Disorders (DSM). The experience of traumatic stress include subtypes of anxiety, depression and disturbance of conduct along with combinations of these symptoms. This may result from events that are less threatening and distressing than those that lead to post-traumatic stress disorder. The fifth edition of the DSM describes in a section titled "Trauma and Stress-Related Disorders" disinhibited social engagement disorder, reactive attachment disorder, acute stress disorder, adjustment disorder, and post-traumatic stress disorder.
Memory and trauma is the deleterious effects that physical or psychological trauma has on memory.
Raymond Monsour Scurfield is an American professor emeritus of social work, The University of Southern Mississippi, Gulf Coast. He is in private practice with Rivers Psychotherapy Services in Gulfport MS; and he has been the external clinical consultant to the Biloxi VA Vet Center since 2011. He has been recognized for his expertise in war-related and natural disaster Psychological trauma. He has published books and articles exploring the effects of post traumatic stress disorder (PTSD) in both combat veterans and disaster survivors, including a trilogy of books about war’s impact. The trilogy’s third installment, War Trauma: Lessons Unlearned from Vietnam to Iraq, was published in October 2006. His three newest books are Scurfield, R.M. & Platoni, K.T. (Eds.). War Trauma & Its Wake. Expanding the Circle of Healing. New York & London: Routledge (2012); Scurfield, R.M. & Platoni, K.T. (Eds).Healing War Trauma. A Handbook of Creative Approaches. New York & London (2013); and Faith-Based and Secular Meditation: Everyday and Posttraumatic Applications. Washington, D.C.: NASW Press (2019)(see review on Amazon.com books).

Shell shock is a term coined in World War I by the British psychologist Charles Samuel Myers to describe the type of post-traumatic stress disorder (PTSD) many soldiers were afflicted with during the war. It is a reaction to the intensity of the bombardment and fighting that produced a helplessness appearing variously as panic and being scared, flight, or an inability to reason, sleep, walk or talk.
Remote location stress reaction, in the past commonly known as logging fatigue, is a range of behaviours resulting from the stress of data logging which decrease the operator's working efficiency.

Posttraumatic stress disorder (PTSD) is a cognitive disorder, which may occur after a traumatic event. It is a psychiatric disorder, which may occur across athletes at all levels of sport participation.
Operational stress injury or OSI is a non-clinical, non-medical term referring to a persistent psychological difficulty caused by traumatic experiences or prolonged high stress or fatigue during service as a military member or first responder. The term does not replace any individual diagnoses or disorders, but rather describes a category of mental health concerns linked to the particular challenges that these military members or first responders encounter in their service. There is not yet a single fixed definition. The term was first conceptualized within the Canadian Armed Forces to help foster understanding of the broader mental health challenges faced by military members who have been impacted by traumatic experiences and who face difficulty as a result. OSI encompasses a number of the diagnoses found in the Diagnostic and Statistical Manual of Mental Disorders (DSM) classification system, with the common thread being a linkage to the operational experiences of the afflicted. The term has gained traction outside of the military community as an appropriate way to describe similar challenges suffered by those whose work regularly exposes them to trauma, particularly front line emergency first responders such as but not limited to police, firefighters, paramedics, correctional officers, and emergency dispatchers. The term, at present mostly used within Canada, is increasingly significant in the development of legislation, policy, treatments and benefits in the military and first responder communities.

Post-traumatic stress disorder (PTSD) results after experiencing or witnessing a terrifying event which later leads to mental health problems. This disorder has always existed but has only been recognized as a psychological disorder within the past forty years. Before receiving its official diagnosis in 1980, when it was published in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-lll), Post-traumatic stress disorder was more commonly known as soldier's heart, irritable heart, or shell shock. Shell shock and war neuroses were coined during World War I when symptoms began to be more commonly recognized among many of the soldiers that had experienced similar traumas. By World War II, these symptoms were identified as combat stress reaction or battle fatigue. In the first edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-I), post-traumatic stress disorder was called gross stress reaction which was explained as prolonged stress due to a traumatic event. Upon further study of this disorder in World War II veterans, psychologists realized that their symptoms were long-lasting and went beyond an anxiety disorder. Thus, through the effects of World War II, post-traumatic stress disorder was eventually recognized as an official disorder in 1980.