Related Research Articles

The endometrium is the inner epithelial layer, along with its mucous membrane, of the mammalian uterus. It has a basal layer and a functional layer: the basal layer contains stem cells which regenerate the functional layer. The functional layer thickens and then is shed during menstruation in humans and some other mammals, including apes, Old World monkeys, some species of bat, the elephant shrew and the Cairo spiny mouse. In most other mammals, the endometrium is reabsorbed in the estrous cycle. During pregnancy, the glands and blood vessels in the endometrium further increase in size and number. Vascular spaces fuse and become interconnected, forming the placenta, which supplies oxygen and nutrition to the embryo and fetus. The speculated presence of an endometrial microbiota has been argued against.

The uterus or womb is the organ in the reproductive system of most female mammals, including humans, that accommodates the embryonic and fetal development of one or more embryos until birth. The uterus is a hormone-responsive sex organ that contains glands in its lining that secrete uterine milk for embryonic nourishment.

The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth. Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.

The chorion is the outermost fetal membrane around the embryo in mammals, birds and reptiles (amniotes). It develops from an outer fold on the surface of the yolk sac, which lies outside the zona pellucida, known as the vitelline membrane in other animals. In insects it is developed by the follicle cells while the egg is in the ovary.

Pre-eclampsia is a disorder of pregnancy characterized by the onset of high blood pressure and often a significant amount of protein in the urine. When it arises, the condition begins after 20 weeks of pregnancy. In severe cases of the disease there may be red blood cell breakdown, a low blood platelet count, impaired liver function, kidney dysfunction, swelling, shortness of breath due to fluid in the lungs, or visual disturbances. Pre-eclampsia increases the risk of undesirable as well as lethal outcomes for both the mother and the fetus including preterm labor. If left untreated, it may result in seizures at which point it is known as eclampsia.

Gestational hypertension or pregnancy-induced hypertension (PIH) is the development of new hypertension in a pregnant woman after 20 weeks' gestation without the presence of protein in the urine or other signs of pre-eclampsia. Gestational hypertension is defined as having a blood pressure greater than 140/90 on two occasions at least 6 hours apart.

The trophoblast is the outer layer of cells of the blastocyst. Trophoblasts are present four days after fertilization in humans. They provide nutrients to the embryo and develop into a large part of the placenta. They form during the first stage of pregnancy and are the first cells to differentiate from the fertilized egg to become extraembryonic structures that do not directly contribute to the embryo. After blastulation, the trophoblast is contiguous with the ectoderm of the embryo and is referred to as the trophectoderm. After the first differentiation, the cells in the human embryo lose their totipotency because they can no longer form a trophoblast. They become pluripotent stem cells.
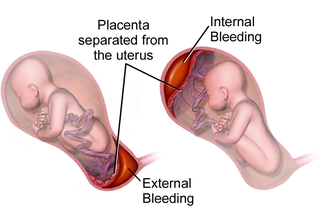
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
Soluble fms-like tyrosine kinase-1 is a tyrosine kinase protein with antiangiogenic properties. A non-membrane associated splice variant of VEGF receptor 1 (Flt-1), sFlt-1 binds the angiogenic factors VEGF and PlGF, reducing blood vessel growth through reduction of free VEGF and PlGF concentrations. In humans, sFlt-1 is important in the regulation of blood vessel formation in diverse tissues, including the kidneys, cornea, and uterus. Abnormally high levels of sFlt-1 have been implicated in the pathogenesis of preeclampsia.

The decidua is the modified mucosal lining of the uterus that forms every month, in preparation for pregnancy. It is shed off each month when there is no fertilised egg to support. The decidua is under the influence of progesterone. Endometrial cells become highly characteristic. The decidua forms the maternal part of the placenta and remains for the duration of the pregnancy. After birth the decidua is shed together with the placenta.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.

Placentation refers to the formation, type and structure, or arrangement of the placenta. The function of placentation is to transfer nutrients, respiratory gases, and water from maternal tissue to a growing embryo, and in some instances to remove waste from the embryo. Placentation is best known in live-bearing mammals (theria), but also occurs in some fish, reptiles, amphibians, a diversity of invertebrates, and flowering plants. In vertebrates, placentas have evolved more than 100 times independently, with the majority of these instances occurring in squamate reptiles.

"Cytotrophoblast" is the name given to both the inner layer of the trophoblast or the cells that live there. It is interior to the syncytiotrophoblast and external to the wall of the blastocyst in a developing embryo.
Placental insufficiency or utero-placental insufficiency is the failure of the placenta to deliver sufficient nutrients to the fetus during pregnancy, and is often a result of insufficient blood flow to the placenta. The term is also sometimes used to designate late decelerations of fetal heart rate as measured by cardiotocography or an NST, even if there is no other evidence of reduced blood flow to the placenta, normal uterine blood flow rate being 600mL/min.

Implantation, also known as nidation is the stage in the embryonic development of mammals in which the blastocyst hatches, attaches, adheres, and invades into the wall of the female's uterus. Implantation is the first stage of gestation, and, when successful, the female is considered to be pregnant. In a woman, an implanted embryo is detected by the presence of increased levels of human chorionic gonadotropin (hCG) in a pregnancy test. The implanted embryo will receive oxygen and nutrients in order to grow.

Decidualization is a process that results in significant changes to cells of the endometrium in preparation for, and during, pregnancy. This includes morphological and functional changes to endometrial stromal cells (ESCs), the presence of decidual white blood cells (leukocytes), and vascular changes to maternal arteries. The sum of these changes results in the endometrium changing into a structure called the decidua. In humans, the decidua is shed during childbirth.

Uterine glands or endometrial glands are tubular glands, lined by ciliated columnar epithelium, found in the functional layer of the endometrium that lines the uterus. Their appearance varies during the menstrual cycle. During the proliferative phase, uterine glands appear long due to estrogen secretion by the ovaries. During the secretory phase, the uterine glands become very coiled with wide lumens and produce a glycogen-rich secretion known as histotroph or uterine milk. This change corresponds with an increase in blood flow to spiral arteries due to increased progesterone secretion from the corpus luteum. During the pre-menstrual phase, progesterone secretion decreases as the corpus luteum degenerates, which results in decreased blood flow to the spiral arteries. The functional layer of the uterus containing the glands becomes necrotic, and eventually sloughs off during the menstrual phase of the cycle.

A placental disease is any disease, disorder, or pathology of the placenta.

The fetal membranes are the four extraembryonic membranes, associated with the developing embryo, and fetus in humans and other mammals. They are the amnion, chorion, allantois, and yolk sac. The amnion and the chorion are the chorioamniotic membranes that make up the amniotic sac which surrounds and protects the embryo. The fetal membranes are four of six accessory organs developed by the conceptus that are not part of the embryo itself, the other two are the placenta, and the umbilical cord.
Extravillous trophoblasts(EVTs), are one form of differentiated trophoblast cells of the placenta. They are invasive mesenchymal cells which function to establish critical tissue connection in the developing placental-uterine interface. EVTs derive from progenitor cytotrophoblasts (CYTs), as does the other main trophoblast subtype, syncytiotrophoblast (SYN). They are sometimes called intermediate trophoblast.
References
- ↑ Pijnenborg, R.; Vercruysse, L. (March 2008). "Shifting Concepts of the Fetal–Maternal Interface: A Historical Perspective". Placenta. 29: 20–25. doi:10.1016/j.placenta.2007.09.006. PMID 17967487.
- ↑ Buttner, Robert; Lee, Jessica; Cadogan, Mike (October 2020). "News: De-eponymizing Anatomical Terminology". Emergency Medicine News. 42 (10): 29–30. doi:10.1097/01.EEM.0000719076.90290.60.
- 1 2 Schneider, H.; Moser, R. W. (April 2016). "Classics revisited. Raissa Nitabuch, on the uteroplacental circulation and the fibrinous membrane". Placenta. 40: 34–39. doi:10.1016/j.placenta.2016.02.011. ISSN 1532-3102. PMID 27016781.