Related Research Articles
Care in the Community is a British policy of deinstitutionalisation, treating and caring for physically and mentally disabled people in their homes rather than in an institution. Institutional care was the target of widespread criticism during the 1960s and 1970s, but it was not until 1983 that the government of Margaret Thatcher adopted a new policy of care after the Audit Commission published a report called 'Making a Reality of Community Care' which outlined the advantages of domiciliary care.
Sir John Peebles Arbuthnott, PPRSE, FRCPSG, FMedSci, FRCPath was a Scottish microbiologist who was Principal of the University of Strathclyde. He succeeded Lord Wilson of Tillyorn as President of The Royal Society of Edinburgh in October 2011 and was succeeded by Dame Jocelyn Bell Burnell in October 2014.

The Convention of Scottish Local Authorities (COSLA) is the national association of Scottish councils and acts as an employers' association for its 32 member authorities.

NHS Wales is the publicly-funded healthcare system in Wales, and one of the four systems which make up the National Health Service in the United Kingdom.

The East of England Ambulance Service NHS Trust (EEAST) is an NHS trust responsible for providing National Health Service (NHS) ambulance services in the counties of Bedfordshire, Cambridgeshire, Essex, Hertfordshire, Norfolk and Suffolk, in the East of England region. These consist of approximately 6.2 million people across an area of 7,500 square miles (19,000 km2).
The National electronic Library for Health (NeLH) was a digital library service provided by the NHS for healthcare professionals and the public between 1998 and 2006. It briefly became the National Library for Health and elements of it continue to this day as NHS Evidence, managed by the National Institute for Health and Care Excellence, and a range of services provided by Health Education England's Library and Knowledge Service Leads.

The National Health Service (NHS) is the publicly funded healthcare system in England, and one of the four National Health Service systems in the United Kingdom. It is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde. Primarily funded by the government from general taxation, and overseen by the Department of Health and Social Care, the NHS provides healthcare to all legal English residents and residents from other regions of the UK, with most services free at the point of use for most people. The NHS also conducts research through the National Institute for Health and Care Research (NIHR).

The National Health Service (NHS) is the umbrella term for the publicly funded healthcare systems of the United Kingdom, comprising the NHS in England, NHS Scotland and NHS Wales. Health and Social Care in Northern Ireland was created separately and is often locally referred to as "the NHS". The original three systems were established in 1948 as part of major social reforms following the Second World War. The founding principles were that services should be comprehensive, universal and free at the point of delivery—a health service based on clinical need, not ability to pay. Each service provides a comprehensive range of health services, provided without charge for people ordinarily resident in the United Kingdom apart from dental treatment and optical care. In England, NHS patients have to pay prescription charges; some, such as those aged over 60, or those on certain state benefits, are exempt.

Tropical diseases, especially malaria and tuberculosis, have long been a public health problem in Kenya. In recent years, infection with the human immunodeficiency virus (HIV), which causes acquired immune deficiency syndrome (AIDS), also has become a severe problem. Estimates of the incidence of infection differ widely.
Examples of health care systems of the world, sorted by continent, are as follows.

Public Health England (PHE) was an executive agency of the Department of Health and Social Care in England which began operating on 1 April 2013 to protect and improve health and wellbeing and reduce health inequalities. Its formation came as a result of the reorganisation of the National Health Service (NHS) in England outlined in the Health and Social Care Act 2012. It took on the role of the Health Protection Agency, the National Treatment Agency for Substance Misuse and a number of other health bodies. It was an executive agency of the Department of Health and Social Care, and a distinct delivery organisation with operational autonomy.
Healthcare in Malawi and its limited resources are inadequate to fully address factors plaguing the population, including infant mortality and the very high burden of diseases, especially HIV/AIDS, malaria and tuberculosis.

Women's health in India can be examined in terms of multiple indicators, which vary by geography, socioeconomic standing and culture. To adequately improve the health of women in India multiple dimensions of wellbeing must be analysed in relation to global health averages and also in comparison to men in India. Health is an important factor that contributes to human wellbeing and economic growth.

NHS England, formerly the NHS Commissioning Board, is an executive non-departmental public body of the Department of Health and Social Care. It oversees the budget, planning, delivery and day-to-day operation of the commissioning side of the National Health Service in England as set out in the Health and Social Care Act 2012. It directly commissions NHS general practitioners, dentists, optometrists and some specialist services. The Secretary of State publishes annually a document known as the NHS mandate which specifies the objectives which the Board should seek to achieve. National Health Service Regulations are published each year to give legal force to the mandate.
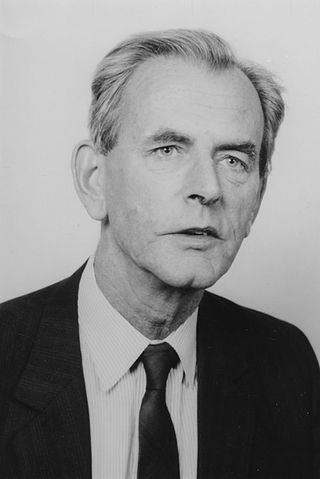
Brian Abel-Smith was a British economist and expert adviser and one of the most influential figures of the twentieth century in shaping health and social welfare. In Britain, his research for the Guillebaud committee in 1956 proved that the NHS provided extremely good value for money and deserved more investment. From the 1960s he was one of a new breed of special advisers to Labour government ministers – helping Richard Crossman, Barbara Castle and David Ennals to reconfigure the NHS, set up Resource Allocation Working Party, and the Black Inquiry into Health Inequalities. Internationally, he steered the development of health services in over 50 countries. He was a key WHO and EEC adviser, intimately involved in setting the agenda for global campaigns such as Health for All by the year 2000.
Healthcare in Essex is now the responsibility of six clinical commissioning groups: Basildon and Brentwood, Mid Essex, North East Essex, Southend, Thurrock and West Essex.
The NHS internal market was established by the National Health Service and Community Care Act 1990, to separate the roles of purchasers and providers within the National Health Service in the United Kingdom. Previously, healthcare was provided by regional health authorities which were given a budget to run hospitals and community health services in their area. The Health and Social Care Act 2012 was intended to open up the internal market to external competition. The 2019 NHS Long Term Plan called for the establishment of integrated care systems across England by 2021, effectively ending the internal market.
In England, a sustainability and transformation plan (STP) is a non-statutory requirement which promotes integrated provision of healthcare, including purchasing and commissioning, within each geographical area of the National Health Service. The plans were introduced in 2016 but by 2018 had been overtaken by progress towards integrated care systems.
Healthcare in Hertfordshire was the responsibility of the Herts Valleys, East, and North Hertfordshire clinical commissioning groups until July 2022.
The NHS Long Term Plan, also known as the NHS 10-Year Plan is a document published by NHS England on 7 January 2019, which sets out its priorities for healthcare over the next 10 years and shows how the NHS funding settlement will be used. It was published by NHS England chief executive Simon Stevens and Prime Minister Theresa May. The plan marked the official abandonment of the policy of competition in the English NHS, which was established by the Health and Social Care Act 2012. Integrated care systems are to be created across England by 2021, Clinical Commissioning Groups are to be merged and NHS England with NHS Improvement appear to be merging, unofficially, though this is all to happen without actually repealing the legislation.
References
- ↑ Royal Commission on the NHS Chapter 3. HMSO. July 1979. ISBN 0-10-176150-3 . Retrieved 18 May 2015.
- ↑ Holland, Prof Walter (2013). Improving Health Services. Edward Elgar Publishing Ltd. ISBN 978-1-78347-018-1.
Gatrell, A.C. (2002) Geographies of Health: an Introduction, Oxford: Blackwell.