Botulinum toxin, or botulinum neurotoxin, is a neurotoxic protein produced by the bacterium Clostridium botulinum and related species. It prevents the release of the neurotransmitter acetylcholine from axon endings at the neuromuscular junction, thus causing flaccid paralysis. The toxin causes the disease botulism. The toxin is also used commercially for medical and cosmetic purposes. Botulinum toxin is an acetylcholine release inhibitor and a neuromuscular blocking agent.
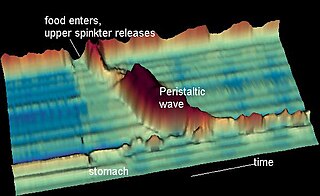
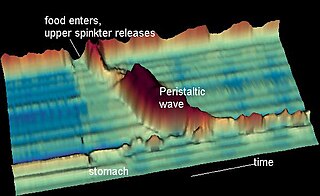
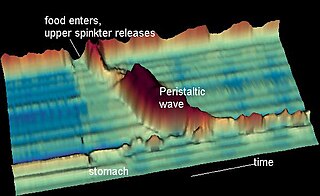
Peristalsis is a type of intestinal motility, characterized by radially symmetrical contraction and relaxation of muscles that propagate in a wave down a tube, in an anterograde direction. Peristalsis is progression of coordinated contraction of involuntary circular muscles, which is preceded by a simultaneous contraction of the longitudinal muscle and relaxation of the circular muscle in the lining of the gut.

The esophagus, oesophagus, or œsophagus all ; pl.: ( e)(œ)sophagi or (œ)sophaguses), colloquially known also as the food pipe, food tube, or gullet, is an organ in vertebrates through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. The esophagus is a fibromuscular tube, about 25 cm (10 in) long in adults, that travels behind the trachea and heart, passes through the diaphragm, and empties into the uppermost region of the stomach. During swallowing, the epiglottis tilts backwards to prevent food from going down the larynx and lungs. The word oesophagus is from Ancient Greek οἰσοφάγος (oisophágos), from οἴσω (oísō), future form of φέρω + ἔφαγον.

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of achalasia exist, but this is neither fully understood, nor agreed upon.
An esophageal motility disorder (EMD) is any medical disorder resulting from dysfunction of the coordinated movement of esophagus, which causes dysphagia.
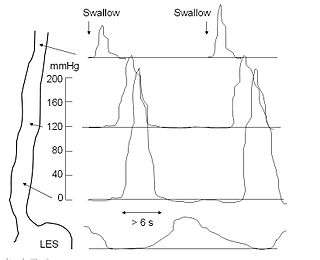
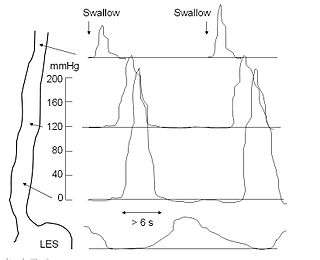
An esophageal motility study (EMS) or esophageal manometry is a test to assess motor function of the upper esophageal sphincter (UES), esophageal body and lower esophageal sphincter (LES).

An anal fissure is a break or tear in the skin of the anal canal. Anal fissures may be noticed by bright red anal bleeding on toilet paper and undergarments, or sometimes in the toilet. If acute they are painful after defecation, but with chronic fissures, pain intensity often reduces and becomes cyclical.
Burping is the release of gas from the upper digestive tract of animals through the mouth. It is always audible.

The inferior pharyngeal constrictor muscle is a skeletal muscle of the neck. It is the thickest of the three outer pharyngeal muscles. It arises from the sides of the cricoid cartilage and the thyroid cartilage. It is supplied by the vagus nerve. It is active during swallowing, and partially during breathing and speech. It may be affected by Zenker's diverticulum.

Oropharyngeal dysphagia is the inability to empty material from the oropharynx into the esophagus as a result of malfunction near the esophagus. Oropharyngeal dysphagia manifests differently depending on the underlying pathology and the nature of the symptoms. Patients with dysphagia can experience feelings of food sticking to their throats, coughing and choking, weight loss, recurring chest infections, or regurgitation. Depending on the underlying cause, age, and environment, dysphagia prevalence varies. In research including the general population, the estimated frequency of oropharyngeal dysphagia has ranged from 2 to 16 percent.
Esophageal spasm is a disorder of motility of the esophagus.
Nutcracker esophagus, jackhammer esophagus, or hypercontractile peristalsis, is a disorder of the movement of the esophagus characterized by contractions in the smooth muscle of the esophagus in a normal sequence but at an excessive amplitude or duration. Nutcracker esophagus is one of several motility disorders of the esophagus, including achalasia and diffuse esophageal spasm. It causes difficulty swallowing (dysphagia) with both solid and liquid foods, and can cause significant chest pain; it may also be asymptomatic. Nutcracker esophagus can affect people of any age but is more common in the sixth and seventh decades of life.

Bladder sphincter dyssynergia is a consequence of a neurological pathology such as spinal injury or multiple sclerosis which disrupts central nervous system regulation of the micturition (urination) reflex resulting in dyscoordination of the detrusor muscles of the bladder and the male or female external urethral sphincter muscles. In normal lower urinary tract function, these two separate muscle structures act in synergistic coordination. But in this neurogenic disorder, the urethral sphincter muscle, instead of relaxing completely during voiding, dyssynergically contracts causing the flow to be interrupted and the bladder pressure to rise.
Cricopharyngeal spasms occur in the cricopharyngeus muscle of the pharynx. Cricopharyngeal spasm is an uncomfortable but harmless and temporary disorder.
Cricopharyngeal myotomy is a surgical sectioning of the cricopharyngeus muscle, also known as the upper esophageal sphincter, that has been advocated for the treatment of cricopharyngeal spasm, or cricopharyngeal achalasia, that leads to cervical dysphagia in the clinical setting.

Anismus or dyssynergic defecation is the failure of normal relaxation of pelvic floor muscles during attempted defecation. It can occur in both children and adults, and in both men and women. It can be caused by physical defects or it can occur for other reasons or unknown reasons. Anismus that has a behavioral cause could be viewed as having similarities with parcopresis, or psychogenic fecal retention.
The per-oral endoscopic myotomy, or POEM, is a minimally invasive surgical procedure for the treatment of achalasia wherein the inner circular muscle layer of the lower esophageal sphincter is divided through a submucosal tunnel. This enables food and liquids to pass into the stomach, a process that is impaired in achalasia. The tunnel is created, and the myotomy performed, using a flexible endoscope, meaning the entire procedure can be done without external incisions.
Prof Clare Fowler CBE is a British physician and academic who created the subspecialty of uro-neurology, a medical field that combines urology and neurology. This work was done at the Institute of Neurology, University College London, where she is an emeritus professor.
Esophagogastric junction outflow obstruction (EGJOO) is an esophageal motility disorder characterized by increased pressure where the esophagus connects to the stomach at the lower esophageal sphincter. EGJOO is diagnosed by esophageal manometry. However, EGJOO has a variety of etiologies; evaluating the cause of obstruction with additional testing, such as upper endoscopy, computed tomography, or endoscopic ultrasound may be necessary. When possible, treatment of EGJOO should be directed at the cause of obstruction. When no cause for obstruction is found, observation alone may be considered if symptoms are minimal. Functional EGJOO with significant or refractory symptoms may be treated with pneumatic dilation, per-oral endoscopic myotomy (POEM), or botulinum toxin injection.

Pankaj "Jay" Pasricha is a physician and researcher specializing in gastroenterology and neurogastroenterology. He currently serves as the chair of medicine at the Mayo Clinic in Scottsdale, Arizona. Formerly, he served as the director of the Johns Hopkins Center for Neurogastroenterology and was the founder and co-director of the Amos Food, Body and Mind Center, Vice Chair of Medicine for Innovation and Commercialization in the Johns Hopkins School of Medicine, and Professor of Innovation Management at the Carey Business School.