Related Research Articles

A coma is a deep state of prolonged unconsciousness in which a person cannot be awakened; fails to respond normally to painful stimuli, light, or sound; lacks a normal wake-sleep cycle; and does not initiate voluntary actions. The person may experience respiratory and circulatory problems due to the body's inability to maintain normal bodily functions. People in a coma often require extensive medical care to maintain their health and prevent complications such as pneumonia or blood clots. Coma patients exhibit a complete absence of wakefulness and are unable to consciously feel, speak or move. Comas can be derived by natural causes, or can be medically induced.
Delirium is a specific state of acute confusion attributable to the direct physiological consequence of a medical condition, effects of a psychoactive substance, or multiple causes, which usually develops over the course of hours to days. As a syndrome, delirium presents with disturbances in attention, awareness, and higher-order cognition. People with delirium may experience other neuropsychiatric disturbances, including changes in psychomotor activity, disrupted sleep-wake cycle, emotional disturbances, disturbances of consciousness, or, altered state of consciousness, as well as perceptual disturbances, although these features are not required for diagnosis.
Sedation is the reduction of irritability or agitation by administration of sedative drugs, generally to facilitate a medical procedure or diagnostic procedure. Examples of drugs which can be used for sedation include isoflurane, diethyl ether, propofol, etomidate, ketamine, pentobarbital, lorazepam and midazolam.
The AVPU scale is a system by which a health care professional can measure and record a patient's level of consciousness. It is mostly used in emergency medicine protocols, and within first aid.
An induced coma – also known as a medically induced coma (MIC), barbiturate-induced coma, or drug-induced coma – is a temporary coma brought on by a controlled dose of an anesthetic drug, often a barbiturate such as pentobarbital or thiopental. Other intravenous anesthetic drugs such as midazolam or propofol may be used.
Cognitive disorders (CDs), also known as neurocognitive disorders (NCDs), are a category of mental health disorders that primarily affect cognitive abilities including learning, memory, perception, and problem-solving. Neurocognitive disorders include delirium, mild neurocognitive disorders, and major neurocognitive disorder. They are defined by deficits in cognitive ability that are acquired, typically represent decline, and may have an underlying brain pathology. The DSM-5 defines six key domains of cognitive function: executive function, learning and memory, perceptual-motor function, language, complex attention, and social cognition.

A minimally conscious state or MCS is a disorder of consciousness distinct from persistent vegetative state and locked-in syndrome. Unlike persistent vegetative state, patients with MCS have partial preservation of conscious awareness. MCS is a relatively new category of disorders of consciousness. The natural history and longer term outcome of MCS have not yet been thoroughly studied. The prevalence of MCS was estimated to be 9 times of PVS cases, or between 112,000 and 280,000 in the US by year 2000.

The corneal reflex, also known as the blink reflex or eyelid reflex, is an involuntary blinking of the eyelids elicited by stimulation of the cornea, though it could result from any peripheral stimulus. Stimulation should elicit both a direct and consensual response. The reflex occurs at a rapid rate of 0.1 seconds. The purpose of this reflex is to protect the eyes from foreign bodies and bright lights. The blink reflex also occurs when sounds greater than 40–60 dB are made.
The auditory brainstem response (ABR), also called brainstem evoked response audiometry (BERA) or brainstem auditory evoked potentials (BAEPs) or brainstem auditory evoked responses (BAERs) is an auditory evoked potential extracted from ongoing electrical activity in the brain and recorded via electrodes placed on the scalp. The measured recording is a series of six to seven vertex positive waves of which I through V are evaluated. These waves, labeled with Roman numerals in Jewett and Williston convention, occur in the first 10 milliseconds after onset of an auditory stimulus. The ABR is considered an exogenous response because it is dependent upon external factors.

An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensive care medicine.
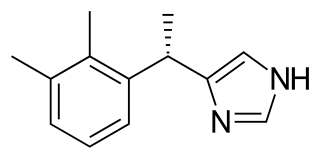
Dexmedetomidine, sold under the trade name Precedex among others, is a drug used in humans for sedation. Veterinarians use dexmedetomidine for similar purposes in treating cats, dogs, and horses. It is also used in humans to treat acute agitation associated with schizophrenia or bipolar I or II disorder.

Dental fear, or dentophobia, is a normal emotional reaction to one or more specific threatening stimuli in the dental situation. However, dental anxiety is indicative of a state of apprehension that something dreadful is going to happen in relation to dental treatment, and it is usually coupled with a sense of losing control. Similarly, dental phobia denotes a severe type of dental anxiety, and is characterised by marked and persistent anxiety in relation to either clearly discernible situations or objects or to the dental setting in general. The term ‘dental fear and anxiety’ (DFA) is often used to refer to strong negative feelings associated with dental treatment among children, adolescents and adults, whether or not the criteria for a diagnosis of dental phobia are met. Dental phobia can include fear of dental procedures, dental environment or setting, fear of dental instruments or fear of the dentist as a person. People with dental phobia often avoid the dentist and neglect oral health, which may lead to painful dental problems and ultimately force a visit to the dentist. The emergency nature of this appointment may serve to worsen the phobia. This phenomenon may also be called the cycle of dental fear. Dental anxiety typically starts in childhood. There is the potential for this to place strains on relationships and negatively impact on employment.
Procedural sedation and analgesia (PSA) is a technique in which a sedating/dissociative medication is given, usually along with an analgesic medication, in order to perform non-surgical procedures on a patient. The overall goal is to induce a decreased level of consciousness while maintaining the patient's ability to breathe on their own. Airway protective reflexes are not compromised by this process and therefore endotracheal intubation is not required. PSA is commonly used in the emergency department, in addition to the operating room.
The National Institutes of Health Stroke Scale, or NIH Stroke Scale (NIHSS), is a tool used by healthcare providers to objectively quantify the impairment caused by a stroke and aid planning post-acute care disposition, though was intended to assess differences in interventions in clinical trials. The NIHSS was designed for the National Institute of Neurological Disorders and Stroke (NINDS) Recombinant Tissue Plasminogen Activator (rt-PA) for Acute Stroke Trial and was first published by neurologist Dr. Patrick Lyden and colleagues in 2001. Prior to the NIHSS, during the late 1980s, several stroke-deficit rating scales were in use.

An altered level of consciousness is any measure of arousal other than normal. Level of consciousness (LOC) is a measurement of a person's arousability and responsiveness to stimuli from the environment. A mildly depressed level of consciousness or alertness may be classed as lethargy; someone in this state can be aroused with little difficulty. People who are obtunded have a more depressed level of consciousness and cannot be fully aroused. Those who are not able to be aroused from a sleep-like state are said to be stuporous. Coma is the inability to make any purposeful response. Scales such as the Glasgow coma scale have been designed to measure the level of consciousness.
Disorders of consciousness are medical conditions that inhibit consciousness. Some define disorders of consciousness as any change from complete self-awareness to inhibited or absent self-awareness and arousal. This category generally includes minimally conscious state and persistent vegetative state, but sometimes also includes the less severe locked-in syndrome and more severe but rare chronic coma. Differential diagnosis of these disorders is an active area of biomedical research. Finally, brain death results in an irreversible disruption of consciousness. While other conditions may cause a moderate deterioration or transient interruption of consciousness, they are not included in this category.
The FOUR Score is a clinical grading scale designed for use by medical professionals in the assessment of patients with impaired level of consciousness. It was developed by Dr. Eelco F.M. Wijdicks and colleagues in Neurocritical care at the Mayo Clinic in Rochester, Minnesota. "FOUR" in this context is an acronym for "Full Outline of UnResponsiveness".
Emergence delirium is a condition in which emergence from general anesthesia is accompanied by psychomotor agitation. Some see a relation to pavor nocturnus while others see a relation to the excitement stage of anesthesia.
Pain stimulus is a technique used by medical personnel for assessing the consciousness level of a person who is not responding to normal interaction, voice commands or gentle physical stimuli. It forms one part of a number of neurological assessments, including the first aid based AVPU scale and the more medically based Glasgow Coma Scale.
The 4 'A's Test (4AT) is a bedside medical scale used to help determine if a person has positive signs for delirium. The 4AT also includes cognitive test items, making it suitable also for use as a rapid test for cognitive impairment.
References
- ↑ Curtis N. Sessler, Mark S. Gosnell, Mary Jo Grap, Gretchen M. Brophy, Pam V. O'Neal, Kimberly A. Keane, Eljim P. Tesoro, and R. K. Elswick "The Richmond Agitation–Sedation Scale", American Journal of Respiratory and Critical Care Medicine, Vol. 166, No. 10 (2002), pp. 1338-1344. doi: 10.1164/rccm.2107138
- ↑ Stawicki SP "Sedation scales: Very useful, very underused", OPUS 12 Scientist, Vol. 1, No. 2 (2007), pp. 10-12.
- ↑ Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, Francis J, Speroff T, Gautam S, Margolin R, Sessler CN, Dittus RS, Bernard GR. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA. 2003 Jun 11;289(22):2983-91.
- ↑ "Monitoring Delirium in the ICU". ICUdelirium.org. Retrieved 2015-04-28.