Related Research Articles

A respiratory therapist is a specialized healthcare practitioner trained in critical care and cardio-pulmonary medicine in order to work therapeutically with people who have acute critical conditions, cardiac and pulmonary disease. Respiratory therapists graduate from a college or university with a degree in respiratory therapy and have passed a national board certifying examination. The NBRC is responsible for credentialing as a CRT, or RRT in the United States. The CBRC is responsible for credentialing as an RRT in Canada.

Cardiopulmonary bypass (CPB) or heart-lung machine also called the pump or CPB pump is a machine that temporarily takes over the function of the heart and lungs during open-heart surgery by maintaining the circulation of blood and oxygen throughout the body. As such it is an extracorporeal device.

Intensive care medicine, usually called critical care medicine, is a medical specialty that deals with seriously or critically ill patients who have, are at risk of, or are recovering from conditions that may be life-threatening. It includes providing life support, invasive monitoring techniques, resuscitation, and end-of-life care. Doctors in this specialty are often called intensive care physicians, critical care physicians, or intensivists.

Extracorporeal membrane oxygenation (ECMO), is a form of extracorporeal life support, providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of oxygen, gas exchange or blood supply (perfusion) to sustain life. The technology for ECMO is largely derived from cardiopulmonary bypass, which provides shorter-term support with arrested native circulation. The device used is a membrane oxygenator, also known as an artificial lung.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.

A cardiovascular perfusionist, clinical perfusionist or perfusiologist, and occasionally a cardiopulmonary bypass doctor or clinical perfusion scientist, is a healthcare professional who operates the cardiopulmonary bypass machine during cardiac surgery and other surgeries that require cardiopulmonary bypass to manage the patient's physiological status. As a member of the cardiovascular surgical team, the perfusionist also known as the clinical perfusionist helps maintain blood flow to the body's tissues as well as regulate levels of oxygen and carbon dioxide in the blood, using a heart–lung machine.

Helen Brooke Taussig was an American cardiologist, working in Baltimore and Boston, who founded the field of pediatric cardiology. She is credited with developing the concept for a procedure that would extend the lives of children born with Tetralogy of Fallot. This concept was applied in practice as a procedure known as the Blalock-Thomas-Taussig shunt. The procedure was developed by Alfred Blalock and Vivien Thomas, who were Taussig's colleagues at the Johns Hopkins Hospital.
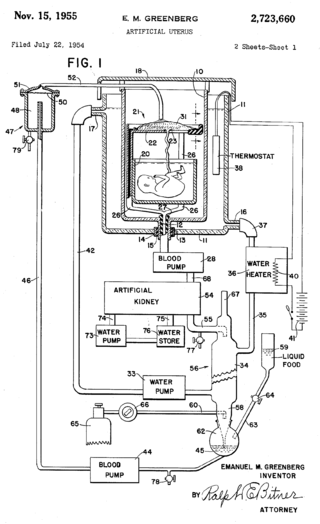
An artificial womb or artificial uterus is a device that would allow for extracorporeal pregnancy, by growing a fetus outside the body of an organism that would normally carry the fetus to term. An artificial uterus, as a replacement organ, would have many applications. It could be used to assist male or female couples in the development of a fetus. This can potentially be performed as a switch from a natural uterus to an artificial uterus, thereby moving the threshold of fetal viability to a much earlier stage of pregnancy. In this sense, it can be regarded as a neonatal incubator with very extended functions. It could also be used for the initiation of fetal development. An artificial uterus could also help make fetal surgery procedures at an early stage an option instead of having to postpone them until term of pregnancy.

Congenital diaphragmatic hernia (CDH) is a birth defect of the diaphragm. The most common type of CDH is a Bochdalek hernia; other types include Morgagni hernia, diaphragm eventration and central tendon defects of the diaphragm. Malformation of the diaphragm allows the abdominal organs to push into the chest cavity, hindering proper lung formation.

Glenfield Hospital, formally known as Glenfield General Hospital, is situated near Glenfield, on the outskirts of Leicester. It is one of England's main hospitals for coronary care and respiratory diseases. It is a tertiary referral university teaching hospital, with a strong international reputation for medical research in cardiac and respiratory health. It is managed by the University Hospitals of Leicester NHS Trust.
Geisinger Medical Center (GMC) is an academic medical center in Danville, Pennsylvania that opened in 1915 as the George F. Geisinger Memorial Hospital. It is the flagship hospital for the Danville-based Geisinger Health System, a primary chain of hospitals and clinics across northeastern and central Pennsylvania.

Morgan Stanley Children's Hospital of NewYork-Presbyterian is a women's and children's hospital at 3959 Broadway, near West 165th Street, in the Washington Heights neighborhood of Manhattan, New York City. It is a part of NewYork-Presbyterian Hospital and the Columbia University Irving Medical Center. The hospital treats patients aged 0–21 from New York City and around the world. The hospital features a dedicated regional ACS designated pediatric Level 1 Trauma Center and is named after financial firm Morgan Stanley, which largely funded its construction through philanthropy.

Rainbow Babies & Children's Hospital is a pediatric acute care children's teaching hospital located in Cleveland, Ohio. It is affiliated with Case Western Reserve University School of Medicine and has a neonatal intensive care unit (NICU), pediatric intensive care unit (PICU), and level 1 pediatric trauma center.
An oxygenator is a medical device that is capable of exchanging oxygen and carbon dioxide in the blood of human patients during surgical procedures that may necessitate the interruption or cessation of blood flow in the body, a critical organ or great blood vessel. These organs can be the heart, lungs or liver, while the great vessels can be the aorta, pulmonary artery, pulmonary veins or vena cava.

The bidirectional Glenn (BDG) shunt, or bidirectional cavopulmonary anastomosis, is a surgical technique used in pediatric cardiac surgery procedure used to temporarily improve blood oxygenation for patients with a congenital cardiac defect resulting in a single functional ventricle. Creation of a bidirectional shunt reduces the amount of blood volume that the heart needs to pump at the time of surgical repair with the Fontan procedure.

Redmond P. Burke is an American congenital heart surgeon, innovator, software developer, author, inventor, and founder of The Congenital Heart Institute at Miami Children's Hospital in Miami, Florida. He starred in the ABC pilot television show The Miracle Workers. Burke has been recognized as one of the world's most innovative surgeons, and for his use of information technology to improve surgical outcomes.
Cardiothoracic anesthesiology is a subspeciality of the medical practice of anesthesiology, devoted to the preoperative, intraoperative, and postoperative care of adult and pediatric patients undergoing cardiothoracic surgery and related invasive procedures.

Pulmonary hypoplasia is an incomplete development of the lungs, resulting in an abnormally low number or small size of bronchopulmonary segments or alveoli. A congenital malformation, most often occurs secondary to other fetal abnormalities that interfere with normal development of the lungs. Primary (idiopathic) pulmonary hypoplasia is rare and usually not associated with other maternal or fetal abnormalities.

The Extracorporeal Life Support Organization (ELSO) is a non profit organization established in 1989 supporting health care professionals and scientists who are involved in extracorporeal membrane oxygenation (ECMO). ELSO maintains a registry of both facilities and specialists trained to provide ECMO services. ELSO also maintains registry information that is used to support clinical research, support regulatory agencies, and support individual ELSO centers. ELSO provides educational programs for active centers as well as for facilities who may be involved in the transfer of patients to higher levels of care.
Extracorporeal cardiopulmonary resuscitation is a method of cardiopulmonary resuscitation (CPR) that passes the patient's blood through a machine in a process to oxygenate the blood supply. A portable extracorporeal membrane oxygenation (ECMO) device is used as an adjunct to standard CPR. A patient who is deemed to be in cardiac arrest refractory to CPR has percutaneous catheters inserted into the femoral vein and artery. Theoretically, the application of ECPR allows for the return of cerebral perfusion in a more sustainable manner than with external compressions alone. By attaching an ECMO device to a person who has acutely undergone cardiovascular collapse, practitioners can maintain end-organ perfusion whilst assessing the potential reversal of causal pathology, with the goal of improving long-term survival and neurological outcomes.
References
- 1 2 "Faculty Memoir Project: Robert Bartlett". University of Michigan . Retrieved May 7, 2014.
- ↑ Coran, A., Caldamone, A., Adzick, N. S., Krummel, T., Laberge, J., Shamberger, R. (2012). Pediatric Surgery: Expert Consult - Online and Print, 7th Ed.: Volume 2. Elsevier Health Sciences. p. 8. ISBN 978-0323091619.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ↑ Chauhan, S., Subin, S. (2011). "Extracorporeal membrane oxygenation, an anesthesiologist's perspective: Physiology and principles. Part 1". Annals of Cardiac Anaesthesia . 14 (3): 218–229. doi: 10.4103/0971-9784.84030 . PMID 21860197 . Retrieved May 7, 2014.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ "Dr. Robert Bartlett, Surgeon and Inventor: Reflections On A Life In Medicine". Ann Arbor District Library . Retrieved May 7, 2014.
- ↑ "The Robert Bartlett Professorship in Pediatric Surgery". University of Michigan Medical School . Retrieved May 7, 2014.
- ↑ Brunk, Doug (April 2006). "Physician Writers Share Their Zeal for Storytelling". Clinical Psychiatry News. Archived from the original on May 8, 2014. Retrieved May 7, 2014.
- ↑ "About Us: Executive and Operational Management". CytoSorbents Corporation. Retrieved May 7, 2014.
- ↑ "About Us: Our Team". CytoSorbents Corporation. Retrieved May 7, 2014.
- ↑ "Section on Surgery Awards" (PDF). American Academy of Pediatrics . Retrieved May 7, 2014.