A melanocytic nevus is usually a noncancerous condition of pigment-producing skin cells. It is a type of melanocytic tumor that contains nevus cells. Some sources equate the term mole with "melanocytic nevus", but there are also sources that equate the term mole with any nevus form.

Nevus is a nonspecific medical term for a visible, circumscribed, chronic lesion of the skin or mucosa. The term originates from nævus, which is Latin for "birthmark"; however, a nevus can be either congenital or acquired. Common terms, including mole, birthmark, and beauty mark, are used to describe nevi, but these terms do not distinguish specific types of nevi from one another.

Hyperkeratosis is thickening of the stratum corneum, often associated with the presence of an abnormal quantity of keratin, and also usually accompanied by an increase in the granular layer. As the corneum layer normally varies greatly in thickness in different sites, some experience is needed to assess minor degrees of hyperkeratosis.

A dysplastic nevus or atypical mole is a nevus (mole) whose appearance is different from that of common moles. In 1992, the NIH recommended that the term "dysplastic nevus" be avoided in favor of the term "atypical mole". An atypical mole may also be referred to as an atypical melanocytic nevus, atypical nevus, B-K mole, Clark's nevus, dysplastic melanocytic nevus, or nevus with architectural disorder.
Keratoderma is a hornlike skin condition.

The congenital melanocytic nevus is a type of melanocytic nevus found in infants at birth. This type of birthmark occurs in an estimated 1% of infants worldwide; it is located in the area of the head and neck 15% of the time.

Becker's nevus is a benign skin disorder predominantly affecting males. The nevus can be present at birth, but more often shows up around puberty. It generally first appears as an irregular pigmentation on the torso or upper arm, and gradually enlarges irregularly, becoming thickened and often hairy (hypertrichosis). The nevus is due to an overgrowth of the epidermis, pigment cells (melanocytes), and hair follicles. This form of nevus was first documented in 1948 by American dermatologist Samuel William Becker (1894–1964).

Nevus of Ota is a hyperpigmentation that occurs on the face, most often appearing on the white of the eye. It also occurs on the forehead, nose, cheek, periorbital region, and temple.

A blue nevus is a type of coloured mole, typically a single well-defined blue-black bump.
Phakomatosis pigmentovascularis is a rare neurocutanous condition where there is coexistence of a capillary malformation with various melanocytic lesions, including dermal melanocytosis, nevus spilus, and nevus of Ota.
Ichthyosis hystrix is a group of rare skin disorders in the ichthyosis family of skin disorders characterized by massive hyperkeratosis with an appearance like spiny scales. This term is also used to refer to a type of epidermal nevi with extensive bilateral distribution.

Nevus lipomatosus (cutaneous) superficialis is characterized by soft, yellowish papules or cerebriform plaques, usually of the buttock or thigh, less often of the ear or scalp, with a wrinkled rather than warty surface. It is usually congenital in origin or appears within the first three decades.

A Spitz nevus is a benign skin lesion. A type of melanocytic nevus, it affects the epidermis and dermis.
Epidermal nevus syndrome is a rare disease that was first described in 1968 and consists of extensive epidermal nevi with abnormalities of the central nervous system (CNS), skeleton, skin, cardiovascular system, genitourinary system and eyes. However, since the syndrome's first description, a broader concept for the "epidermal nevus" syndrome has been proposed, with at least six types being described:
A benign melanocytic nevus is a cutaneous condition characterised by well-circumscribed, pigmented, round or ovoid lesions, generally measuring from 2 to 6 mm in diameter. A benign melanocytic nevus may feature hair or pigmentation as well.
Pseudomelanoma is a cutaneous condition in which melanotic skin lesions clinically resemble a superficial spreading melanoma at the site of a recent shave removal of a melanocytic nevus.
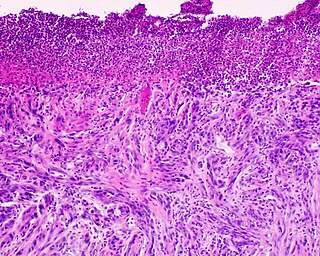
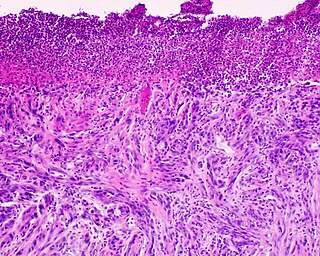
Desmoplastic melanoma is a rare cutaneous condition characterized by a deeply infiltrating type of melanoma with an abundance of fibrous matrix. It usually occurs in the head and neck region of older people with sun-damaged skin. Diagnosis can be difficult as it has a similar appearance to sclerosing melanocytic nevi as well as some nonmelanocytic skin lesions such as scars, fibromas, or cysts.
Walter Russell "Nick" Nickel, M.D. was an American dermatologist who was one of the founders of the field of dermatopathology. He was a co-founder and president of four different professional societies and was the founding chairman of the Division of Dermatology at the University of California, San Diego Medical Center.

An acral nevus is a cutaneous condition of the palms, soles, fingers, or toes, characterized by a skin lesion that is usually macular or only slightly elevated, and may display a uniform brown or dark brown color, often with linear striations.

A pigmented spindle cell nevus is a skin condition characterized by a dark brown to black macule or papule, usually less than 6 mm.