Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.
Schizophrenia is a mental disorder characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucinations, delusions, and disorganized thinking. Other symptoms include social withdrawal, and flat affect. Symptoms typically develop gradually, begin during young adulthood, and in many cases never become resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a psychiatric history that includes the person's reported experiences, and reports of others familiar with the person. To be diagnosed with schizophrenia, the described symptoms need to have been present for at least six months or one month. Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders, anxiety disorders, and obsessive–compulsive disorder.
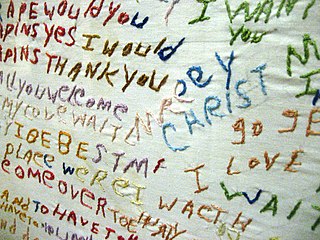
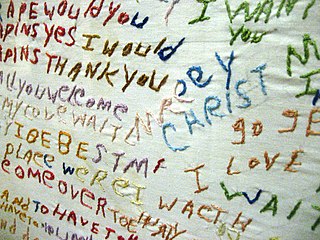
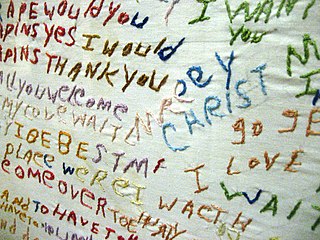
A thought disorder (TD) is a disturbance in cognition which affects language, thought and communication. Psychiatric and psychological glossaries in 2015 and 2017 identified thought disorders as encompassing poverty of ideas, neologisms, paralogia, word salad, and delusions - all disturbances of thought content and form. Two specific terms have been suggested — content thought disorder (CTD) and formal thought disorder (FTD). CTD has been defined as a thought disturbance characterized by multiple fragmented delusions, and the term thought disorder is often used to refer to an FTD: a disruption of the form of thought. Also known as disorganized thinking, FTD results in disorganized speech and is recognized as a major feature of schizophrenia and other psychoses. Disorganized speech leads to an inference of disorganized thought. Thought disorders include derailment, pressured speech, poverty of speech, tangentiality, verbigeration, and thought blocking. One of the first known cases of thought disorders, or specifically OCD as we know it today, was in 1691. John Moore, who was a bishop, had a speech in front of Queen Mary II, about "religious melancholy."
In psychology, alogia is poor thinking inferred from speech and language usage. There may be a general lack of additional, unprompted content seen in normal speech, so replies to questions may be brief and concrete, with less spontaneous speech. This is termed poverty of speech or laconic speech. The amount of speech may be normal but conveys little information because it is vague, empty, stereotyped, overconcrete, overabstract, or repetitive. This is termed poverty of content or poverty of content of speech. Under Scale for the Assessment of Negative Symptoms used in clinical research, thought blocking is considered a part of alogia, and so is increased latency in response.
The mental status examination (MSE) is an important part of the clinical assessment process in neurological and psychiatric practice. It is a structured way of observing and describing a patient's psychological functioning at a given point in time, under the domains of appearance, attitude, behavior, mood and affect, speech, thought process, thought content, perception, cognition, insight, and judgment. There are some minor variations in the subdivision of the MSE and the sequence and names of MSE domains.
The Global Assessment of Functioning (GAF) is a numeric scale used by mental health clinicians and physicians to rate subjectively the social, occupational, and psychological functioning of an individual, i.e., how well one is meeting various problems in living. Scores range from 100 to 1.
Disorganized schizophrenia, or hebephrenia, was a subtype of schizophrenia prior to 2013. Subtypes of schizophrenia were no longer recognized as separate conditions in the DSM 5, published in 2013. The disorder is no longer listed in the 11th revision of the International Classification of Diseases (ICD-11).

Thought broadcasting is a form of delusional condition wherein the individual believes that others can hear their inner thoughts. The person may hold the belief that either those nearby can perceive their thoughts or that their thoughts are being transmitted via mediums, such as television, radio or the internet.
The Positive and Negative Syndrome Scale (PANSS) is a medical scale used for measuring symptom severity of patients with schizophrenia. It was published in 1987 by Stanley Kay, Lewis Opler, and Abraham Fiszbein. It is widely used in the study of antipsychotic therapy. The scale is the "gold standard" for evaluating the effects of psychopharmacological treatments.
Schizophreniform disorder is a mental disorder diagnosed when symptoms of schizophrenia are present for a significant portion of time, but signs of disturbance are not present for the full six months required for the diagnosis of schizophrenia.
Nancy Coover Andreasen is an American neuroscientist and neuropsychiatrist. She currently holds the Andrew H. Woods Chair of Psychiatry at the Roy J. and Lucille A. Carver College of Medicine at the University of Iowa.
Schedules for Clinical Assessment in Neuropsychiatry (SCAN) is a set of tools created by WHO aimed at diagnosing and measuring mental illness that may occur in adult life. It is not constructed explicitly for use with either ICD-10 or DSM-IV but can be used for both systems. The SCAN system was originally called PSE, or Present State Examination, but since version 10 (PSE-10), the commonly accepted name has been SCAN. The current version of SCAN is 2.1.
Grandiose delusions (GD), also known as delusions of grandeur or expansive delusions, are a subtype of delusion that occur in patients with a wide range of psychiatric disorders, including two-thirds of patients in a manic state of bipolar disorder, half of those with schizophrenia, patients with the grandiose subtype of delusional disorder, frequently in narcissistic personality disorder, and a substantial portion of those with substance abuse disorders. GDs are characterized by fantastical beliefs that one is famous, omnipotent, wealthy, or otherwise very powerful. The delusions are generally fantastic and typically have a religious, science fictional, or supernatural theme. There is a relative lack of research into GD, in contrast to persecutory delusions and auditory hallucinations. Around 10% of healthy people experience grandiose thoughts at some point in their lives but do not meet full criteria for a diagnosis of GD.
The Brief Psychiatric Rating Scale (BPRS) is a rating scale which a clinician or researcher may use to measure psychiatric symptoms such as depression, anxiety, hallucinations and unusual behaviour. The scale is one of the oldest, most widely used scales to measure psychotic symptoms and was first published in 1962.
Childhood schizophrenia is similar in characteristics of schizophrenia that develops at a later age, but has an onset before the age of 13 years, and is more difficult to diagnose. Schizophrenia is characterized by positive symptoms that can include hallucinations, delusions, and disorganized speech; negative symptoms, such as blunted affect and avolition and apathy, and a number of cognitive impairments. Differential diagnosis is problematic since several other neurodevelopmental disorders, including autism spectrum disorder, language disorder, and attention deficit hyperactivity disorder, also have signs and symptoms similar to childhood-onset schizophrenia.
Somatic symptom disorder, also known as somatoform disorder, is defined by one or more chronic physical symptoms that coincide with excessive and maladaptive thoughts, emotions, and behaviors connected to those symptoms. The symptoms are not purposefully produced or feigned, and they may or may not coexist with a known medical ailment. Manifestations of Somatic symptom disorder are variable and symptoms can be widespread, specific, and often fluctuate. Somatic symptom disorder corresponds to the way an individual views and reacts to symptoms as rather than the symptoms themselves. Somatic symptom disorder may develop in those who suffer from an existing chronic illness or medical condition.
A religious delusion is defined as a delusion, or fixed belief not amenable to change in light of conflicting evidence, involving religious themes or subject matter. Religious faith, meanwhile, is defined as a belief in God or a religious doctrine in the absence of evidence. Psychologists, scientists, and philosophers have debated the distinction between the two, which is subjective and cultural.
The Scale for the Assessment of Negative Symptoms (SANS) is a rating scale that mental health professionals use to measure negative symptoms in schizophrenia. Negative symptoms are those conspicuous by their absence—lack of concern for one's appearance, and lack of language and communication skills, for example. Nancy Andreasen developed the scale and first published it in 1984. SANS splits assessment into five domains. Within each domain it rates separate symptoms from 0 (absent) to 5 (severe). The scale is closely linked to the Scale for the Assessment of Positive Symptoms (SAPS), which was published a few years later. These tools are available for clinicians and for research.
The Hamilton Anxiety Rating Scale (HAM-A) is a psychological questionnaire used by clinicians to rate the severity of a patient's anxiety. Anxiety can refer to things such as "a mental state...a drive...a response to a particular situation…a personality trait...and a psychiatric disorder." Though it was one of the first anxiety rating scales to be published, the HAM-A remains widely used by clinicians. It was originally published by Max Hamilton in 1959. For clinical purposes, and the purpose of this scale, only severe or improper anxiety is attended to. This scale is considered a "clinical rating" of the extensiveness of anxiety, and is intended for individuals that are "already diagnosed with anxiety neurosis."