Related Research Articles
Chronic pain or chronic pain syndrome is a type of pain that is also known by other titles such as gradual burning pain, electrical pain, throbbing pain, and nauseating pain. This type of pain is sometimes confused with acute pain and can last from three months to several years; various diagnostic manuals such as DSM-5 and ICD-11 have proposed several definitions of chronic pain, but the accepted definition is that it is "pain that lasts longer than the expected period of recovery."
Local anesthesia is any technique to induce the absence of sensation in a specific part of the body, generally for the aim of inducing local analgesia, i.e. local insensitivity to pain, although other local senses may be affected as well. It allows patients to undergo surgical and dental procedures with reduced pain and distress. In many situations, such as cesarean section, it is safer and therefore superior to general anesthesia.

Pain management is an aspect of medicine and health care involving relief of pain in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals provide some pain control in the normal course of their practice, and for the more complex instances of pain, they also call on additional help from a specific medical specialty devoted to pain, which is called pain medicine.
Diabetic neuropathy is various types of nerve damage associated with diabetes mellitus. The most common form, diabetic peripheral neuropathy, affects 30% of all diabetic patients. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from a microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.
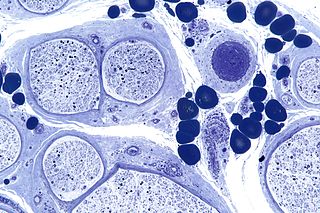
Peripheral neuropathy, often shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerve fibers are affected. Neuropathies affecting motor, sensory, or autonomic nerve fibers result in different symptoms. More than one type of fiber may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

A transcutaneous electrical nerve stimulation is a device that produces mild electric current to stimulate the nerves for therapeutic purposes. TENS, by definition, covers the complete range of transcutaneously applied currents used for nerve excitation, but the term is often used with a more restrictive intent—namely, to describe the kind of pulses produced by portable stimulators used to reduce pain. The unit is usually connected to the skin using two or more electrodes which are typically conductive gel pads. A typical battery-operated TENS unit is able to modulate pulse width, frequency, and intensity. Generally, TENS is applied at high frequency (>50 Hz) with an intensity below motor contraction or low frequency (<10 Hz) with an intensity that produces motor contraction. More recently, many TENS units use a mixed frequency mode which alleviates tolerance to repeated use. Intensity of stimulation should be strong but comfortable with greater intensities, regardless of frequency, producing the greatest analgesia. While the use of TENS has proved effective in clinical studies, there is controversy over which conditions the device should be used to treat.
A microcurrent electrical neuromuscular stimulator or MENS is a device used to send weak electrical signals into the body. Such devices apply extremely small microamp [uA] electrical currents to the tissues using electrodes placed on the skin. One microampere [uA] is 1 millionth of an ampere and the uses of MENS are distinct from those of "TENS" which runs at one milliamp [mA] or one thousandth of an amp.

Hyperalgesia is an abnormally increased sensitivity to pain, which may be caused by damage to nociceptors or peripheral nerves and can cause hypersensitivity to stimulus. Prostaglandins E and F are largely responsible for sensitizing the nociceptors. Temporary increased sensitivity to pain also occurs as part of sickness behavior, the evolved response to infection.
Postherpetic neuralgia (PHN) is neuropathic pain that occurs due to damage to a peripheral nerve caused by the reactivation of the varicella zoster virus. PHN is defined as pain in a dermatomal distribution that lasts for at least 90 days after an outbreak of herpes zoster. Several types of pain may occur with PHN including continuous burning pain, episodes of severe shooting or electric-like pain, and a heightened sensitivity to gentle touch which would not otherwise cause pain or to painful stimuli. Abnormal sensations and itching may also occur.
Neuropathic pain is pain caused by a lesion or disease of the somatosensory nervous system. Neuropathic pain may be associated with abnormal sensations called dysesthesia or pain from normally non-painful stimuli (allodynia). It may have continuous and/or episodic (paroxysmal) components. The latter resemble stabbings or electric shocks. Common qualities include burning or coldness, "pins and needles" sensations, numbness and itching.
Neuralgia is pain in the distribution of a nerve or nerves, as in intercostal neuralgia, trigeminal neuralgia, and glossopharyngeal neuralgia.
Sacral nerve stimulation, also termed sacral neuromodulation, is a type of medical electrical stimulation therapy.
Electroanalgesia is a form of analgesia, or pain relief, that uses electricity to ease pain. Electrical devices can be internal or external, at the site of pain (local) or delocalized throughout the whole body. It works by interfering with the electric currents of pain signals, inhibiting them from reaching the brain and inducing a response; different from traditional analgesics, such as opiates which mimic natural endorphins and NSAIDs that help relieve inflammation and stop pain at the source. Electroanalgesia has a lower addictive potential and poses less health threats to the general public, but can cause serious health problems, even death, in people with other electrical devices such as pacemakers or internal hearing aids, or with heart problems.

Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. The diagnosis is largely clinical and can be confirmed with diagnostic nerve blocks. Occasionally imaging and electrophysiology studies aid in the diagnosis. Timely diagnosis is important as untreated chronic nerve compression may cause permanent damage. A surgical nerve decompression can relieve pressure on the nerve but cannot always reverse the physiological changes that occurred before treatment. Nerve injury by a single episode of physical trauma is in one sense an acute compression neuropathy but is not usually included under this heading, as chronic compression takes a unique pathophysiological course.
Neurostimulation is the purposeful modulation of the nervous system's activity using invasive or non-invasive means. Neurostimulation usually refers to the electromagnetic approaches to neuromodulation.
Chemotherapy-induced peripheral neuropathy (CIPN) is a nerve-damaging side effect of antineoplastic agents in the common cancer treatment, chemotherapy. CIPN afflicts between 30% and 40% of patients undergoing chemotherapy. Antineoplastic agents in chemotherapy are designed to eliminate rapidly dividing cancer cells, but they can also damage healthy structures, including the peripheral nervous system. CIPN involves various symptoms such as tingling, pain, and numbness in the hands and feet. These symptoms can impair activities of daily living, such as typing or dressing, reduce balance, and increase risk of falls and hospitalizations. They can also give cause to reduce or discontinue chemotherapy. Researchers have conducted clinical trials and studies to uncover the various symptoms, causes, pathogenesis, diagnoses, risk factors, and treatments of CIPN.
Interventional pain management or interventional pain medicine is a medical subspecialty defined by the National Uniforms Claims Committee (NUCC) as, " invasive interventions such as the discipline of medicine devoted to the diagnosis and treatment of pain related disorders principally with the application of interventional techniques in managing sub acute, chronic, persistent, and intractable pain, independently or in conjunction with other modalities of treatment". Medicare Payment Advisory Commission (MedPAC) defined interventional techniques as, "minimally invasive procedures including, percutaneous precision needle placement, with placement of drugs in targeted areas or ablation of targeted nerves; and some surgical techniques such as laser or endoscopic diskectomy, intrathecal infusion pumps and spinal cord stimulators, for the diagnosis and management of chronic, persistent or intractable pain". Minimally invasive interventions such as facet joint injections, nerve blocks, neuroaugmentation, vertebroplasty, kyphoplasty, nucleoplasty, endoscopic discectomy, and implantable drug delivery systems are utilized in managing subacute or chronic pain.
Occipital nerve stimulation (ONS), also called peripheral nerve stimulation (PNS) of the occipital nerves, is used to treat chronic migraine patients who have failed to respond to pharmaceutical treatments.
Neuromodulation is "the alteration of nerve activity through targeted delivery of a stimulus, such as electrical stimulation or chemical agents, to specific neurological sites in the body". It is carried out to normalize – or modulate – nervous tissue function. Neuromodulation is an evolving therapy that can involve a range of electromagnetic stimuli such as a magnetic field (rTMS), an electric current, or a drug instilled directly in the subdural space. Emerging applications involve targeted introduction of genes or gene regulators and light (optogenetics), and by 2014, these had been at minimum demonstrated in mammalian models, or first-in-human data had been acquired. The most clinical experience has been with electrical stimulation.
Peripheral mononeuropathy is a nerve related disease where a single nerve, that is used to transport messages from the brain to the peripheral body, is diseased or damaged. Peripheral neuropathy is a general term that indicates any disorder of the peripheral nervous system. The name of the disorder itself can be broken down in order to understand this better; peripheral: in regard to peripheral neuropathy, refers to outside of the brain and spinal cord; neuro: means nerve related; -pathy; means disease. Peripheral mononeuropathy is a disorder that links to Peripheral Neuropathy, as it only effects a single peripheral nerve rather than several damaged or diseased nerves throughout the body. Healthy peripheral nerves are able to “carry messages from the brain and spinal cord to muscles, organs, and other body tissues”.
References
- ↑ Katholi BR, Daghstani SS, Banez GA, Brady KK (2014). "Noninvasive treatments for pediatric complex regional pain syndrome: a focused review". PM&R. 6 (10): 926–33. doi: 10.1016/j.pmrj.2014.04.007 . PMID 24780851.
- ↑ Harrison, Pam (11 Jan 2016). "Scrambler Therapy Benefit in Cancer-Related Neuropathic Pain". Medscape (WebMD LLC). Retrieved 24 January 2016.
- 1 2 Pachman, DR; Watson, JC; Loprinzi, CL (December 2014). "Therapeutic strategies for cancer treatment related peripheral neuropathies". Current Treatment Options in Oncology. 15 (4): 567–80. doi:10.1007/s11864-014-0303-7. PMID 25119581. S2CID 22944576.
- ↑ Rivera, E., & Cianfrocca, M. (2015). "Overview of neuropathy associated with taxanes for the treatment of metastatic breast cancer". Cancer Chemotherapy and Pharmacology. 75 (4): 659–670. doi:10.1007/s00280-014-2607-5. PMC 4365177 . PMID 25596818.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Majithia, N; Smith, TJ; Coyne, PJ; Abdi, S; Pachman, DR; Lachance, D; Shelerud, R; Cheville, A; Basford, JR; Farley, D; O'Neill, C; Ruddy, KJ; Sparadeo, F; Beutler, A; Loprinzi, CL (June 2016). "Scrambler Therapy for the management of chronic pain". Supportive Care in Cancer. 24 (6): 2807–14. doi:10.1007/s00520-016-3177-3. PMC 4973603 . PMID 27041741.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Smith, Thomas J.; Wang, Eric J.; Loprinzi, Charles L. (13 July 2023). "Cutaneous Electroanalgesia for Relief of Chronic and Neuropathic Pain". New England Journal of Medicine. 389 (2): 158–164. doi:10.1056/NEJMra2110098. PMID 37437145. S2CID 259843656.
- ↑ Jin, Y; Kim, D; Hur, J; Myung, SK (October 2022). "Efficacy of Scrambler Therapy for Management of Chronic Pain: A Meta-Analysis of Randomized Controlled Trials". Pain Physician. 25 (7): E931–E939. PMID 36288579.
- ↑ Anson, Pat (9 April 2014). "Inventor of Calmare Scrambler Tries to Block Sales". National Pain Report.
- ↑ Serafini, G., Marineo, G. and Sabato, A.F. (2000). "'Scrambler therapy': a new option in neuropathic pain treatment?". The Pain Clinic. 12 (4): 287–298. doi:10.1163/156856900750233785.
{{cite journal}}: CS1 maint: multiple names: authors list (link)