| Secretin-cholecystokinin test | |
|---|---|
| Medical diagnostics | |
| Purpose | assess the function of both the pancreas and gall bladder |
The secretin-cholecystokinin test (aka Secretin-CCK test, Secretin-Pancreozymin test [1] ) is a combination of the secretin test and the cholecystokinin test and is used to assess the function of both the pancreas and gall bladder.

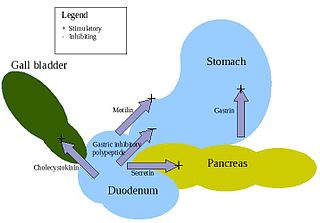
Secretin is a hormone that regulates water homeostasis throughout the body and influences the environment of the duodenum by regulating secretions in the stomach, pancreas, and liver. It is a peptide hormone produced in the S cells of the duodenum, which are located in the intestinal glands. In humans, the secretin peptide is encoded by the SCT gene.

Cholecystokinin is a peptide hormone of the gastrointestinal system responsible for stimulating the digestion of fat and protein. Cholecystokinin, officially called pancreozymin, is synthesized and secreted by enteroendocrine cells in the duodenum, the first segment of the small intestine. Its presence causes the release of digestive enzymes and bile from the pancreas and gallbladder, respectively, and also acts as a hunger suppressant.

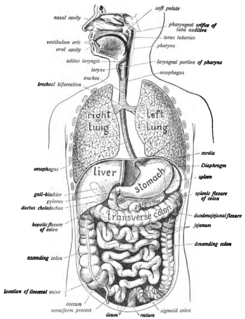
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdominal cavity behind the stomach.
Cholecystokinin, a hormone secreted by the APUD cells located in the proximal mucosa of the small intestine is administered intravenously, this stimulates the pancreatic secretion of the digestive enzymes amylase, trypsin, and lipase. These are measured by a catheter placed in the duodenum. Cholecystokinin also stimulates the flow of bile and causes the gall bladder to contract and thus determine if the gall bladder is emptying properly. It also affects the esophageal sphincter and the sphincter of Oddi by reducing contraction as well as increasing motility (movement) of the stomach and intestine. The CCK test may be administered in conjunction with an ultrasound test to visually monitor gall bladder contraction. While the test is usually administered in a supine position Dr. William Smedley of Wilkes Barre, Pennsylvania has detected previously missed gallbladder abnormalities by administering the test in an erect position. [2] [3] [4]
APUD cells constitute a group of apparently unrelated endocrine cells, which were named by the scientist A.G.E. Pearse, who developed the APUD concept in the early 1960s. These cells share the common function of secreting a low molecular weight polypeptide hormone. There are several different types which secrete the hormones secretin, cholecystokinin and several others. The name is derived from an acronym, referring to the following:
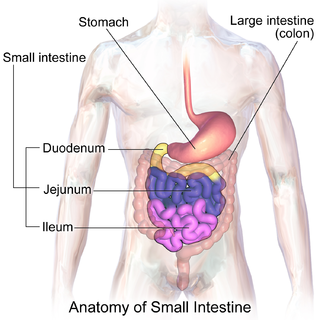
The small intestine or small bowel is the part of the gastrointestinal tract between the stomach and the large intestine, and is where most of the end absorption of food takes place. The small intestine has three distinct regions – the duodenum, jejunum, and ileum. The duodenum is the shortest part of the small intestine and is where preparation for absorption begins. It also receives bile and pancreatic juice through the pancreatic duct, controlled by the sphincter of Oddi. The primary function of the small intestine is the absorption of nutrients and minerals from food, using small finger-like protrusions called villi.
Amylase is an enzyme that catalyses the hydrolysis of starch into sugars. Amylase is present in the saliva of humans and some other mammals, where it begins the chemical process of digestion. Foods that contain large amounts of starch but little sugar, such as rice and potatoes, may acquire a slightly sweet taste as they are chewed because amylase degrades some of their starch into sugar. The pancreas and salivary gland make amylase to hydrolyse dietary starch into disaccharides and trisaccharides which are converted by other enzymes to glucose to supply the body with energy. Plants and some bacteria also produce amylase. As diastase, amylase is the first enzyme to be discovered and isolated. Specific amylase proteins are designated by different Greek letters. All amylases are glycoside hydrolases and act on α-1,4-glycosidic bonds.
The concentration and output of bicarbonate with the secretin-CCK test is similar to what has been observed with the standard secretin test . The secretin-induced rapid flow of water results in lower and often unreliable enzyme concentrations. CCK also induces gallbladder contraction and the release of bile, which may further dilute enzyme concentrations. As a result, the quantification of total enzyme output (units/min) must be determined through continuous collection of duodenal fluid with or without the use of perfusion markers. Measurement of more than one enzyme (i.e. amylase, lipase, and tryptase) and bicarbonate may improve sensitivity since some patients may possess deficiencies of one parameter and not the others .
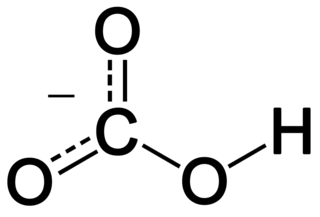
In inorganic chemistry, bicarbonate is an intermediate form in the deprotonation of carbonic acid. It is a polyatomic anion with the chemical formula HCO−
3.

In vertebrates, the gallbladder is a small hollow organ where bile is stored and concentrated before it is released into the small intestine. In humans, the pear-shaped gallbladder lies beneath the liver, although the structure and position of the gallbladder can vary significantly among animal species. It receives and stores bile, produced by the liver, via the common hepatic duct and releases it via the common bile duct into the duodenum, where the bile helps in the digestion of fats.

Bile or gall is a dark green to yellowish brown fluid, produced by the liver of most vertebrates, that aids the digestion of lipids in the small intestine. In humans, bile is produced continuously by the liver, and stored and concentrated in the gallbladder. After eating, this stored bile is discharged into the duodenum. The composition of hepatic bile is 97% water, 0.7% bile salts, 0.2% bilirubin, 0.51% fats, and 200 meq/l inorganic salts.
One study reviewed the relative diagnostic value of enzyme and bicarbonate concentrations compared with enzyme output in 363 secretin-CCK tests . The investigators also evaluated the requirement for perfusion markers to accurately quantify volume, and the validity of a shortened sampling time (first 20 minutes). Only 60 percent of volume was recovered with the duodenal aspiration tube, suggesting that marker perfusion to correct for distal loss of secretion is important to accurately quantify volume.
Using a trypsin output <50 U/kg/h as the reference standard, measurement of enzyme concentration alone misclassified approximately 10 percent of patients. Use of a shortened collection time misclassified approximately 4 percent of patients. The authors concluded that this was an unacceptably high rate of misclassification and that the standard prolonged collection of fluid using a perfusion marker must be performed to accurately measure exocrine function.

Trypsin is a serine protease from the PA clan superfamily, found in the digestive system of many vertebrates, where it hydrolyzes proteins. Trypsin is formed in the small intestine when its proenzyme form, the trypsinogen produced by the pancreas, is activated. Trypsin cleaves peptide chains mainly at the carboxyl side of the amino acids lysine or arginine, except when either is followed by proline. It is used for numerous biotechnological processes. The process is commonly referred to as trypsin proteolysis or trypsinisation, and proteins that have been digested/treated with trypsin are said to have been trypsinized. Trypsin was discovered in 1876 by Wilhelm Kühne.