Related Research Articles

Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.
Sedation is the reduction of irritability or agitation by administration of sedative drugs, generally to facilitate a medical procedure or diagnostic procedure. Examples of drugs which can be used for sedation include isoflurane, diethyl ether, propofol, etomidate, ketamine, pentobarbital, lorazepam and midazolam.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients.

Anesthesiology, anaesthesiology, or anaesthesia is the medical specialty concerned with the total perioperative care of patients before, during and after surgery. It encompasses anesthesia, intensive care medicine, critical emergency medicine, and pain medicine. A physician specialized in anesthesiology is called an anesthesiologist, anaesthesiologist, or anaesthetist, depending on the country. In some countries, the terms are synonymous, while in other countries they refer to different positions, and anesthetist is only used for non-physicians, such as nurse anesthetists.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory of the experience, it is also possible for victims to have awareness with explicit recall, where they can remember the events related to their surgery.
Postoperative nausea and vomiting (PONV) is the phenomenon of nausea, vomiting, or retching experienced by a patient in the postanesthesia care unit (PACU) or within 24 hours following a surgical procedure. PONV affects about 10% of the population undergoing general anaesthesia each year. PONV can be unpleasant and lead to a delay in mobilization and food, fluid, and medication intake following surgery.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

Remifentanil, marketed under the brand name Ultiva is a potent, short-acting synthetic opioid analgesic drug. It is given to patients during surgery to relieve pain and as an adjunct to an anaesthetic. Remifentanil is used for sedation as well as combined with other medications for use in general anesthesia. The use of remifentanil has made possible the use of high-dose opioid and low-dose hypnotic anesthesia, due to synergism between remifentanil and various hypnotic drugs and volatile anesthetics.
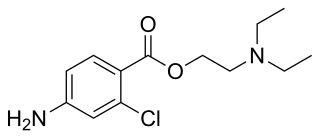
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.

Methoxyflurane, sold under the brand name Penthrox among others, is an inhaled medication primarily used to reduce pain following trauma. It may also be used for short episodes of pain as a result of medical procedures. Onset of pain relief is rapid and of a short duration. Use is only recommended with direct medical supervision.
Veterinary anesthesia is anesthesia performed on non-human animals by a veterinarian or a Registered Veterinary Technician. Anesthesia is used for a wider range of circumstances in animals than in people, due to animals' inability to cooperate with certain diagnostic or therapeutic procedures. Veterinary anesthesia includes anesthesia of the major species: dogs, cats, horses, cattle, sheep, goats, and pigs, as well as all other animals requiring veterinary care such as birds, pocket pets, and wildlife.
Procedural sedation and analgesia (PSA) is a technique in which a sedating/dissociative medication is given, usually along with an analgesic medication, in order to perform non-surgical procedures on a patient. The overall goal is to induce a decreased level of consciousness while maintaining the patient's ability to breathe on their own. Airway protective reflexes are not compromised by this process and therefore endotracheal intubation is not required. PSA is commonly used in the emergency department, in addition to the operating room.

Twilight anesthesia is an anesthetic technique where a mild dose of sedation is applied to induce anxiolysis, hypnosis, and anterograde amnesia. The patient is not unconscious, but sedated. During surgery or other medical procedures, the patient is under what is known as a "twilight state", where the patient is relaxed and "sleepy", able to follow simple directions by the doctor, and is responsive. Generally, twilight anesthesia causes the patient to forget the surgery and the time right after. It is used for a variety of surgical procedures and for various reasons. Just like regular anesthesia, twilight anesthesia is designed to help a patient feel more comfortable and to minimize pain associated with the procedure being performed and to allow the medical practitioner to practice without interruptions.

Patient-controlled analgesia (PCA) is any method of allowing a person in pain to administer their own pain relief. The infusion is programmable by the prescriber. If it is programmed and functioning as intended, the machine is unlikely to deliver an overdose of medication. Providers must always observe the first administration of any PCA medication which has not already been administered by the provider to respond to allergic reactions.
Oral sedation dentistry is a medical procedure involving the administration of sedative drugs via an oral route, generally to facilitate a dental procedure and reduce patients anxiety related to the experience. Oral sedation is one of the available methods of conscious sedation dentistry, along with inhalation sedation and conscious intravenous sedation. Benzodiazepines are commonly used, specifically triazolam. Triazolam is commonly selected for its rapid onset and limited duration of effect. An initial dose is usually taken approximately one hour before the dental appointment. Treatment may include additional dosing on the night proceeding the procedure, to mitigate anxiety-related insomnia. The procedure is generally recognized as safe, with the effective dosages being below levels sufficient to impair breathing.
The following outline is provided as an overview of and topical guide to anesthesia:
Total intravenous anesthesia (TIVA) refers to the intravenous administration of anesthetic agents to induce a temporary loss of sensation or awareness. The first study of TIVA was done in 1872 using chloral hydrate, and the common anesthetic agent propofol was licensed in 1986. TIVA is currently employed in various procedures as an alternative technique of general anesthesia in order to improve post-operative recovery.

Caudal anaesthesia is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults it is used for chronic low back pain management.

Ciprofol is a novel 2,6-disubstituted phenol derivative that is used for the intravenous induction of general anesthesia. A short-acting and highly selective γ-aminobutyric acid agonist, ciprofol is 4–6 times more potent than other phenol derivatives such as propofol or fospropofol.
References
- ↑ Patients’ satisfaction with sedoanalgesia versus subarachnoid analgesia in endourology. Department of Anaesthesia and Intensive Care, Faculty of Medicine, Al Azhar University, Cairo, Egypt. Egyptian Journal of Anaesthesia Volume 27, Issue 3, July 2011, Pages 151–155
- ↑ Triantafillidis, JK; Merikas, E; Nikolakis, D; Papalois, AE (28 January 2013). "Sedation in gastrointestinal endoscopy". World Journal of Gastroenterology. 19 (4): 405–11. doi: 10.3748/wjg.v19.i4.463 . PMC 3558570 . PMID 23382625.