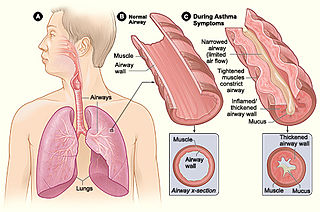
Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. These may occur a few times a day or a few times per week. Depending on the person, asthma symptoms may become worse at night or with exercise.

Chlamydia pneumoniae is a species of Chlamydia, an obligate intracellular bacterium that infects humans and is a major cause of pneumonia. It was known as the Taiwan acute respiratory agent (TWAR) from the names of the two original isolates – Taiwan (TW-183) and an acute respiratory isolate designated AR-39. Briefly, it was known as Chlamydophila pneumoniae, and that name is used as an alternate in some sources. In some cases, to avoid confusion, both names are given.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.
A wheeze is a clinical symptom of a continuous, coarse, whistling sound produced in the respiratory airways during breathing. For wheezes to occur, some part of the respiratory tree must be narrowed or obstructed, or airflow velocity within the respiratory tree must be heightened. Wheezing is commonly experienced by persons with a lung disease; the most common cause of recurrent wheezing is asthma, though it can also be a symptom of lung cancer, congestive heart failure, and certain types of heart diseases.
Acute severe asthma, also known as status asthmaticus, is an acute exacerbation of asthma that does not respond to standard treatments of bronchodilators (inhalers) and corticosteroids. Asthma is caused by multiple genes, some having protective effect, with each gene having its own tendency to be influenced by the environment although a genetic link leading to acute severe asthma is still unknown. Symptoms include chest tightness, rapidly progressive dyspnea, dry cough, use of accessory respiratory muscles, fast and/or labored breathing, and extreme wheezing. It is a life-threatening episode of airway obstruction and is considered a medical emergency. Complications include cardiac and/or respiratory arrest. The increasing prevalence of atopy and asthma remains unexplained but may be due to infection with respiratory viruses.
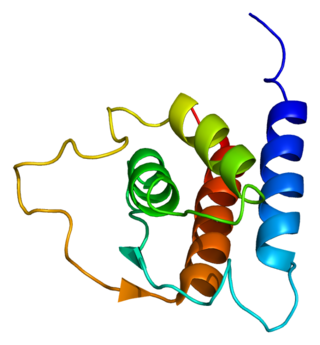
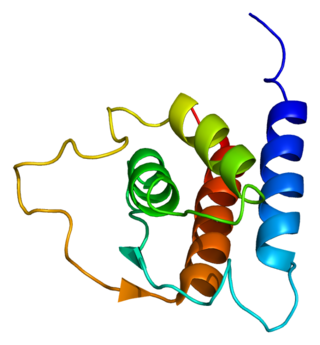
Interleukin 13 (IL-13) is a protein that in humans is encoded by the IL13 gene. IL-13 was first cloned in 1993 and is located on chromosome 5q31.1 with a length of 1.4kb. It has a mass of 13 kDa and folds into 4 alpha helical bundles. The secondary structural features of IL-13 are similar to that of Interleukin 4 (IL-4); however it only has 25% sequence identity to IL-4 and is capable of IL-4 independent signaling. IL-13 is a cytokine secreted by T helper type 2 (Th2) cells, CD4 cells, natural killer T cell, mast cells, basophils, eosinophils and nuocytes. Interleukin-13 is a central regulator in IgE synthesis, goblet cell hyperplasia, mucus hypersecretion, airway hyperresponsiveness, fibrosis and chitinase up-regulation. It is a mediator of allergic inflammation and different diseases including asthma.
Feline asthma is a common allergic respiratory disease in cats, affecting at least one percent of all adult cats worldwide. It is a chronic progressive disease for which there is no cure. Common symptoms include wheezing, coughing, labored breathing and potentially life-threatening bronchoconstriction. There is conjecture that the disease has become more common due to increased exposure to industrial pollutants. Feline asthma can also be attributed to lung damage caused by long-term exposure to second-hand smoke.

Interleukin 33 (IL-33) is a protein that in humans is encoded by the IL33 gene.
Reslizumab is a humanized monoclonal antibody against human interleukin-5 (IL-5). Reslizumab binds specifically to IL-5, a key cytokine responsible for the differentiation, maturation, recruitment and activation of human eosinophils. By binding to human IL-5, it blocks its biological function; consequently survival and activity of eosinophils are reduced. The benefits with reslizumab are its ability to reduce the exacerbation rate and improve lung function and asthma-related quality of life in patients with severe eosinophilic asthma and with at least one previous asthma exacerbation in the preceding year. The most common side effects are increased blood creatine phosphokinase, myalgia and anaphylactic reactions.
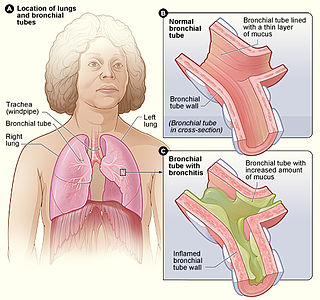
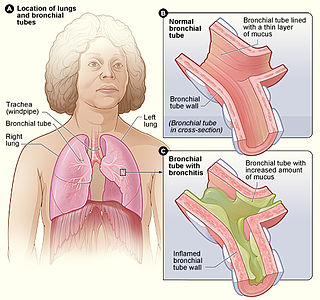
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include; asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.

Interleukin-17A is a protein that in humans is encoded by the IL17A gene. In rodents, IL-17A used to be referred to as CTLA8, after the similarity with a viral gene.

In medicine, exhaled nitric oxide (eNO) can be measured in a breath test for asthma and other respiratory conditions characterized by airway inflammation. Nitric oxide (NO) is a gaseous molecule produced by certain cell types in an inflammatory response. The fraction of exhaled NO (FENO) is a promising biomarker for the diagnosis, follow-up and as a guide to therapy in adults and children with asthma. The breath test has recently become available in many well-equipped hospitals in developed countries, although its exact role remains unclear.
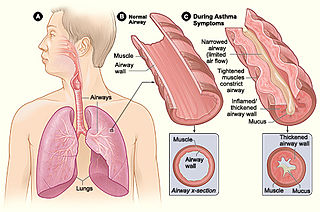
Asthma is a common pulmonary condition defined by chronic inflammation of respiratory tubes, tightening of respiratory smooth muscle, and episodes of bronchoconstriction. The Centers for Disease Control and Prevention estimate that 1 in 11 children and 1 in 12 adults have asthma in the United States of America. According to the World Health Organization, asthma affects 235 million people worldwide. There are two major categories of asthma: allergic and non-allergic. The focus of this article will be allergic asthma. In both cases, bronchoconstriction is prominent.
Dame Margaret Elizabeth Turner-Warwick was a British medical doctor and thoracic specialist. She was the first woman president of the Royal College of Physicians (1989–1992) and, later, chairman of the Royal Devon and Exeter Health Care NHS Trust (1992–1995).

Sir Peter John Barnes, FRCP, FCCP, FMedSci, FRS is a British respiratory scientist and clinician, a specialist in the mechanisms and treatment of asthma and chronic obstructive pulmonary disease (COPD). He was Margaret Turner-Warwick Professor of Thoracic Medicine at the National Heart & Lung Institute, previous head of respiratory medicine at Imperial College and honorary consultant physician at the Royal Brompton Hospital London. He is one of the most highly cited scientists in the world
Clare Margaret Lloyd is a Professor of Medicine and Vice Dean for Institutional Affairs at Imperial College London. She investigates allergic immunity in early life.
Jane C. Davies is a British physician who is Professor of Paediatric Respirology at Imperial College School of Medicine. She is an Honorary Consultant at the Royal Brompton and Harefield NHS Foundation Trust.
Rosemary Jane Boyton is a British immunologist who is Head of Lung Immunology and Adult Infectious Disease at Imperial College London. She works on the molecular immunology of infectious, allergic and autoimmune inflammation. She holds an honorary consultant position at the Royal Brompton Hospital, where she specialises in lung infection.
Scarlett Bellamy is an American public health researcher who is a Professor of the Department of Epidemiology and Biostatistics at Drexel University. At Drexel she is Associate Dean of Diversity, Inclusion and Faculty Development.