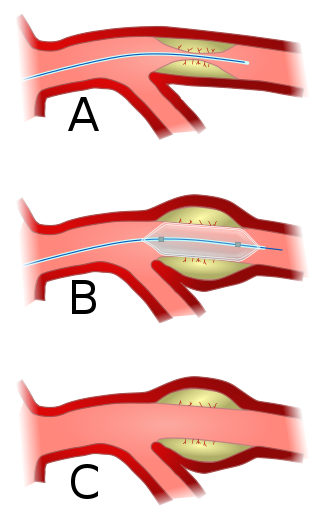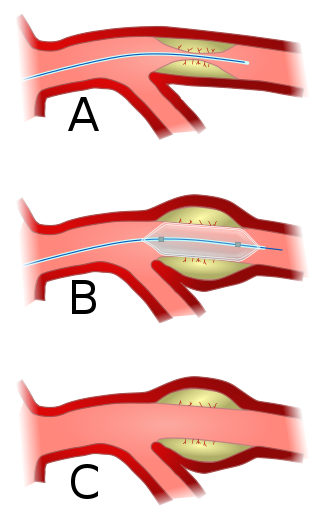
Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. A deflated balloon attached to a catheter is passed over a guide-wire into the narrowed vessel and then inflated to a fixed size. The balloon forces expansion of the blood vessel and the surrounding muscular wall, allowing an improved blood flow. A stent may be inserted at the time of ballooning to ensure the vessel remains open, and the balloon is then deflated and withdrawn. Angioplasty has come to include all manner of vascular interventions that are typically performed percutaneously.

Aortic stenosis is the narrowing of the exit of the left ventricle of the heart, such that problems result. It may occur at the aortic valve as well as above and below this level. It typically gets worse over time. Symptoms often come on gradually with a decreased ability to exercise often occurring first. If heart failure, loss of consciousness, or heart related chest pain occur due to AS the outcomes are worse. Loss of consciousness typically occurs with standing or exercising. Signs of heart failure include shortness of breath especially when lying down, at night, or with exercise, and swelling of the legs. Thickening of the valve without narrowing is known as aortic sclerosis.

A thoracic aortic aneurysm is an aortic aneurysm that presents primarily in the thorax.

Left ventricular hypertrophy (LVH) is thickening of the heart muscle of the left ventricle of the heart, that is, left-sided ventricular hypertrophy and resulting increased left ventricular mass.

A pneumonectomy is a surgical procedure to remove a lung. It was first successfully performed in 1933 by Dr. Evarts Graham. This is not to be confused with a lobectomy or segmentectomy, which only removes one part of the lung.

Carotid endarterectomy is a surgical procedure used to reduce the risk of stroke from carotid artery stenosis. In endarterectomy, the surgeon opens the artery and removes the plaque. The plaque forms and thickens the inner layer of the artery, or intima, hence the name of the procedure which simply means removal of part of the internal layers of the artery.

Carotid artery stenosis is a narrowing or constriction of any part of the carotid arteries, usually caused by atherosclerosis.

Vascular disease is a class of diseases of the vessels of the circulatory system in the body, including blood vessels – the arteries and veins, and the lymphatic vessels. Vascular disease is a subgroup of cardiovascular disease. Disorders in this vast network of blood and lymph vessels can cause a range of health problems that can sometimes become severe, and fatal. Coronary heart disease for example, is the leading cause of death for men and women in the United States.
The Canadian Cardiovascular Society (CCS) is the national voice for cardiovascular physicians and scientists in Canada. The CCS is a membership organization that represents more than 1,800 professionals in the cardiovascular field. Its mission is to promote cardiovascular health and care through knowledge translation, professional development and leadership in health policy.

Intima–media thickness (IMT), also called intimal medial thickness, is a measurement of the thickness of tunica intima and tunica media, the innermost two layers of the wall of an artery. The measurement is usually made by external ultrasound and occasionally by internal, invasive ultrasound catheters. Measurements of the total wall thickness of blood vessels can also be done using other imaging modalities.
David L. Reich is an American academic anesthesiologist, who has been President & Chief Operating Officer of The Mount Sinai Hospital, and President of Mount Sinai Queens, since October 2013.
Jonathan L. Halperin is an American cardiologist and the author of Bypass (ISBN 0-89586-509-2), among the most comprehensive works on the subject of coronary artery bypass surgery. In addition, he is the Robert and Harriet Heilbrunn Professor of Medicine at The Mount Sinai School of Medicine as well as Director of Clinical Cardiology in the Zena and Michael A. Wierner Cardiovascular Institute at The Mount Sinai Medical Center, both in New York City. Halperin was the principal cardiologist responsible for both the design and execution of the multi-center Stroke Prevention in Atrial Fibrillation (SPAF) clinical trials, funded by the National Institutes of Health, which helped develop antithrombotic strategies to prevent stroke, and he subsequently directed the SPORTIF clinical trials, which evaluated the first oral direct thrombin inhibitor for prevention of stroke in patients with atrial fibrillation.
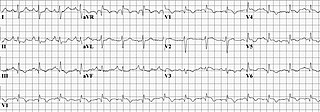
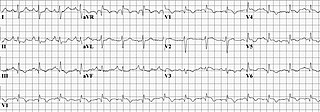
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.

Cardiac imaging refers to minimally invasive imaging of the heart using ultrasound, magnetic resonance imaging (MRI), computed tomography (CT), or nuclear medicine (NM) imaging with PET or SPECT. These cardiac techniques are otherwise referred to as echocardiography, Cardiac MRI, Cardiac CT, Cardiac PET and Cardiac SPECT including myocardial perfusion imaging.
The Revised Cardiac Risk Index (RCRI) is a tool used to estimate a patient's risk of perioperative cardiac complications. The RCRI and similar clinical prediction tools are derived by looking for an association between preoperative variables (e.g., patient's age, type of surgery, comorbid diagnoses, or laboratory data) and the risk for cardiac complications in a cohort of surgical patients (the "derivation cohort"). Variables that have independent predictive value in a logistic regression analysis are incorporated into the risk index. Ideally, the accuracy and validity of the risk index is then tested in a separate cohort (the "validation cohort"). In 1977 Goldman, et al., developed the first cardiac risk index, which included nine variables associated with an increased risk of perioperative cardiac complications. This became known as the Original Cardiac Risk Index (or alternatively the Goldman Index). In 1999, Lee et al. published a cardiac risk index derived from 2893 patients and validated in 1422 patients aged ≥ 50 undergoing major noncardiac surgery, which became known as the Revised Cardiac Risk Index (RCRI). Lee identified six independent variables that predicted an increased risk for cardiac complications. A patient's risk for perioperative cardiac complications increased with number of variables that were present.
Right heart strain is a medical finding of right ventricular dysfunction where the heart muscle of the right ventricle (RV) is deformed. Right heart strain can be caused by pulmonary hypertension, pulmonary embolism, RV infarction, chronic lung disease, pulmonic stenosis, bronchospasm, and pneumothorax.
William A. Zoghbi is a Lebanese-American cardiologist. He is Professor of Medicine at the Houston Methodist Institute for Academic Medicine, in Houston Texas, and Weill Cornell Medical College. He holds the Elkins Family Distinguished Chair in Cardiac Health at the Houston Methodist DeBakey Heart & Vascular Center. Zoghbi is the Chairman of the Department of Cardiology at Houston Methodist Hospital. He is a Master of the American College of Cardiology and served as its president in 2012.

George "Rick" Stouffer is an American cardiologist who is Chief of the Division of Cardiology at the University of North Carolina Medical Center, where he is a practicing interventional cardiologist. Stouffer was awarded the Ernest and Hazel Craige Distinguished Professorship of Medicine in 2018; prior to that he was the Henry A. Foscue Distinguished Professor of Medicine. Stouffer is also co-director of the McAllister Heart Institute. He is known for his research regarding inpatient ST elevation myocardial infarctions.
The volume of the heart's left atrium is an important biomarker for cardiovascular physiology and clinical cardiology. It is usually calculated as left atrial volume index in terms of body surface area.
Salvatore Novo is an Italian author, professor and researcher in the field of cardiovascular disease, epidemiology and risk factors of atherosclerosis. He has authored about 550 papers. He is one of the highly cited authors in the field of cardiovascular diseases.