Related Research Articles

A feeding tube is a medical device used to provide nutrition to people who cannot obtain nutrition by mouth, are unable to swallow safely, or need nutritional supplementation. The state of being fed by a feeding tube is called gavage, enteral feeding or tube feeding. Placement may be temporary for the treatment of acute conditions or lifelong in the case of chronic disabilities. A variety of feeding tubes are used in medical practice. They are usually made of polyurethane or silicone. The diameter of a feeding tube is measured in French units. They are classified by the site of insertion and intended use.
Gastric bypass surgery refers to a technique in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass procedures (GBP). Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.
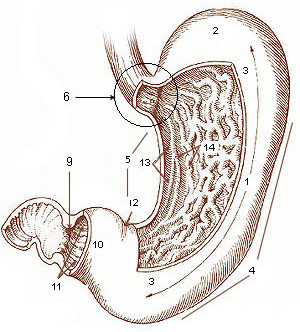
A gastrectomy is a partial or total surgical removal of the stomach.

Percutaneous endoscopic gastrostomy (PEG) is an endoscopic medical procedure in which a tube is passed into a patient's stomach through the abdominal wall, most commonly to provide a means of feeding when oral intake is not adequate. This provides enteral nutrition despite bypassing the mouth; enteral nutrition is generally preferable to parenteral nutrition. The PEG procedure is an alternative to open surgical gastrostomy insertion, and does not require a general anesthetic; mild sedation is typically used. PEG tubes may also be extended into the small intestine by passing a jejunal extension tube through the PEG tube and into the jejunum via the pylorus.

Vertical banded gastroplasty (VBG), also known as stomach stapling, is a form of bariatric surgery for weight control. The VBG procedure involves using a band and staples to create a small stomach pouch. In the bottom of the pouch is an approximate one-centimeter hole through which the pouch contents can flow into the remainder of the stomach and hence on to the remainder of the gastrointestinal tract.
The duodenal switch (DS) procedure, gastric reduction duodenal switch (GRDS), is a weight loss surgery procedure that is composed of a restrictive and a malabsorptive aspect.

A gastrostomy is the creation of an artificial external opening into the stomach for nutritional support or gastric decompression. Typically this would include an incision in the patient's epigastrium as part of a formal operation. When originally devised over a century ago the procedure was completed through open surgery using the Stamm technique. It can be performed through surgical approach, percutaneous approach by interventional radiology, percutaneous endoscopic gastrostomy (PEG) or percutaneous ultrasound gastrostomy (PUG).

A laparoscopic adjustable gastric band, commonly called a lap-band, A band, or LAGB, is an inflatable silicone device placed around the top portion of the stomach to treat obesity, intended to decrease food consumption.

Gastric antral vascular ectasia (GAVE) is an uncommon cause of chronic gastrointestinal bleeding or iron deficiency anemia. The condition is associated with dilated small blood vessels in the pyloric antrum, which is a distal part of the stomach. The dilated vessels result in intestinal bleeding. It is also called watermelon stomach because streaky long red areas that are present in the stomach may resemble the markings on watermelon.
Sleeve gastrectomy or vertical sleeve gastrectomy, is a surgical weight-loss procedure, typically performed laparoscopically, in which approximately 75 - 85% of the stomach is removed, along the greater curvature, which leaves a cylindrical, or "sleeve"-shaped stomach the size of a banana. Weight loss is affected not only through the reduction of the organ's size, but by the removal of the portion of it that produces ghrelin, the hormone that stimulates appetite. Patients can lose 50-70 percent of excess weight over the course of the two years that follow the surgery. The procedure is irreversible, though in some uncommon cases, patients can regain the lost weight, via resumption of poor dietary habits, or dilation of the stomach over time, which can require gastric sleeve revision surgery to either repair the sleeve or convert it to another type of weight loss method that may produce better results, such as a gastric bypass or duodenal switch.

Endoscopic foreign body retrieval refers to the removal of ingested objects from the esophagus, stomach and duodenum by endoscopic techniques. It does not involve surgery, but rather encompasses a variety of techniques employed through the gastroscope for grasping foreign bodies, manipulating them, and removing them while protecting the esophagus and trachea. It is of particular importance with children, people with mental illness, and prison inmates as these groups have a high rate of foreign body ingestion.

A vagotomy is a surgical procedure that involves removing part of the vagus nerve. It is performed in the abdomen.
Bariatric surgery is a medical term for surgical procedures used to manage obesity and obesity-related conditions. Long term weight loss with bariatric surgery may be achieved through alteration of gut hormones, physical reduction of stomach size, reduction of nutrient absorption, or a combination of these. Standard of care procedures include Roux en-Y bypass, sleeve gastrectomy, and biliopancreatic diversion with duodenal switch, from which weight loss is largely achieved by altering gut hormone levels responsible for hunger and satiety, leading to a new hormonal weight set point.
Revision weight loss surgery is a surgical procedure that is performed on patients who have already undergone a form of bariatric surgery, and have either had complications from such surgery or have not achieved significant weight loss results from the initial surgery. Procedures are usually performed laparoscopically, though open surgery may be required if prior bariatric surgery has resulted in extensive scarring.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
A gastric balloon, also known as an intragastric balloon (IGB) or a stomach balloon, is an inflatable medical device that is temporarily placed into the stomach to help reduce weight. It is designed to help provide weight loss when diet and exercise have failed and surgery is not wanted or not recommended for the patient.
A duodenal-jejunal bypass liner, commonly called an EndoBarrier, is an implantable medical device in the form of a thin flexible 60 cm-long tube that creates a physical barrier between ingested food and the duodenum/proximal jejunum. The duodenal-jejunal bypass liner prevents the interaction of food with enzymes and hormones in the proximal intestine to treat type 2 diabetes and obesity. The duodenal-jejunal bypass liner is delivered endoscopically and has been tested on the morbidly obese as well as obese patients with a BMI less than 40, particularly those with difficult-to-manage type 2 diabetes. Despite a handful of serious adverse events such as gastrointestinal bleeding, abdominal pain, and device migration — all resolved with device removal — initial clinical trials have produced promising results in the treatment's ability to improve weight loss and glucose homeostasis outcomes.
Stomach Intestinal Pylorus-Sparing (SIPS) surgery is a type of weight-loss surgery. It was developed in 2013 by two U.S. surgeons, Daniel Cottam from Utah and Mitchell S. Roslin from New York.
In medicine, endoscopic sleeve gastroplasty (ESG) is a minimally-invasive, non-surgical (incisionless), endoscopic weight loss procedure that is part of the field of endoscopic bariatric therapies. To perform ESG, a physician sutures a patient’s stomach into a narrower, smaller tube-like configuration. The result is a more restricted stomach that forces patients to feel fuller sooner, eating fewer calories, which facilitates weight loss.
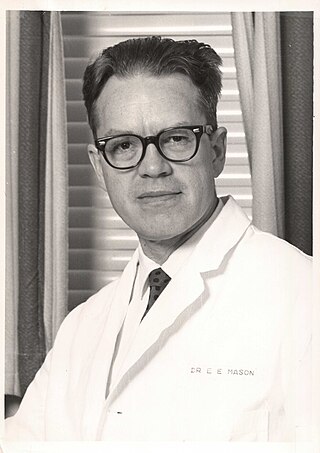
Edward Eaton Mason was an American surgeon, professor, and medical researcher who specialized in obesity surgery. He is known for developing restrictive gastric surgery for morbidly obese patients. Mason introduced the first gastric bypass surgery in 1966 and was the inventor of the first vertical banded gastroplasty surgery in 1980.
References
- 1 2 Woods KE, Abu Dayyeh BK, Thompson CC (2010). "Endoscopic post-bypass revisions". Techniques in Gastrointestinal Endoscopy. 12 (3): 160–166. doi:10.1016/j.tgie.2010.10.002.
- 1 2 Goyal V, Holover S, Garber S (September 2013). "Gastric pouch reduction using StomaphyX in post Roux-en-Y gastric bypass patients does not result in sustained weight loss: a retrospective analysis". Surgical Endoscopy. 27 (9): 3417–20. doi:10.1007/s00464-013-2905-8. PMID 23519492. S2CID 23842803.
- ↑ Ong'uti SK, Ortega G, Onwugbufor MT, Ivey GD, Fullum TM, Tran DD (2013). "Effective weight loss management with endoscopic gastric plication using StomaphyX device: is it achievable?". Surgery for Obesity and Related Diseases. 9 (1): 113–7. doi:10.1016/j.soard.2011.08.025. PMID 22169759.
- ↑ Eid GM, McCloskey CA, Eagleton JK, Lee LB, Courcoulas AP (April 2014). "StomaphyX vs a sham procedure for revisional surgery to reduce regained weight in Roux-en-Y gastric bypass patients : a randomized clinical trial". JAMA Surgery. 149 (4): 372–9. doi: 10.1001/jamasurg.2013.4051 . PMID 24554030.