Related Research Articles

Pulmonology is a medical specialty that deals with diseases involving the respiratory tract. The term is derived from the Latin word pulmō, pulmōnis ("lung") and the Greek suffix -λογία, -logia. Pulmonology is synonymous with pneumology, respirology and respiratory medicine.

Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of lung diseases affecting the interstitium (the tissue and space around the alveoli. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process goes awry and the tissue around the air sacs becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The term ILD is used to distinguish these diseases from obstructive airways diseases.

Respiratory disease, or lung disease, is a medical term that encompasses pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, and the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, acute asthma and lung cancer.
Bronchoalveolar lavage (BAL) [not to be confused with bronchial washing], is a medical procedure in which a bronchoscope is passed through the mouth or nose into the lungs and fluid is squirted into a small part of the lung and then collected for examination. It is typically performed to diagnose lung disease.

Respiratory epithelium, or airway epithelium, is a type of ciliated columnar epithelium found lining most of the respiratory tract as respiratory mucosa, where it serves to moisten and protect the airways. It is not present in the vocal cords of the larynx, or the oropharynx and laryngopharynx, where instead the epithelium is stratified squamous. It also functions as a barrier to potential pathogens and foreign particles, preventing infection and tissue injury by the secretion of mucus and the action of mucociliary clearance.
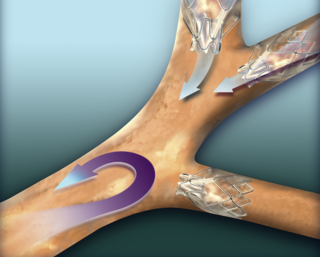
An endobronchial valve(EBV), is an implantable medical device—a small, one-way valve, which is implanted in an airway in the pulmonary system to treat one of several lung conditions. Endobronchial valves are typically implanted using a flexible delivery catheter advanced through a bronchoscope, and thus they are minimally invasive. The valves are also removable if they are not working properly.

Bronchoscopy is an endoscopic technique of visualizing the inside of the airways for diagnostic and therapeutic purposes. An instrument (bronchoscope) is inserted into the airways, usually through the nose or mouth, or occasionally through a tracheostomy. This allows the practitioner to examine the patient's airways for abnormalities such as foreign bodies, bleeding, tumors, or inflammation. Specimens may be taken from inside the lungs. The construction of bronchoscopes ranges from rigid metal tubes with attached lighting devices to flexible optical fiber instruments with realtime video equipment.
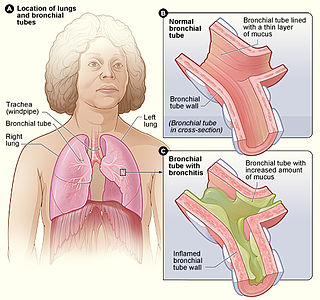
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include; asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.

Pulmonary function test (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a respiratory therapist, physiotherapist, pulmonologist, and/or general practitioner.
Bronchial hyperresponsiveness is a state characterised by easily triggered bronchospasm.

The FEV1/FVC ratio, also called Tiffeneau-Pinelli index, is a calculated ratio used in the diagnosis of obstructive and restrictive lung disease. It represents the proportion of a person's vital capacity that they are able to expire in the first second of forced expiration (FEV1) to the full, forced vital capacity (FVC). The result of this ratio is expressed as FEV1%.
Pulmonary rehabilitation, also known as respiratory rehabilitation, is an important part of the management and health maintenance of people with chronic respiratory disease who remain symptomatic or continue to have decreased function despite standard medical treatment. It is a broad therapeutic concept. It is defined by the American Thoracic Society and the European Respiratory Society as an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities. In general, pulmonary rehabilitation refers to a series of services that are administered to patients of respiratory disease and their families, typically to attempt to improve the quality of life for the patient. Pulmonary rehabilitation may be carried out in a variety of settings, depending on the patient's needs, and may or may not include pharmacologic intervention.

An acute exacerbation of chronic obstructive pulmonary disease (COPD), is a sudden worsening of COPD symptoms including that typically lasts for several days. It may be triggered by an infection with bacteria or viruses or by environmental pollutants. Typically, infections cause 75% or more of the exacerbations; bacteria can roughly be found in 25% of cases, viruses in another 25%, and both viruses and bacteria in another 25%. Airway inflammation is increased during the exacerbation resulting in increased hyperinflation, reduced expiratory air flow and decreased gas exchange.
ENB is a medical procedure utilizing electromagnetic technology designed to localize and guide endoscopic tools or catheters through the bronchial pathways of the lung. Using a virtual, three-dimensional (3D) bronchial map from a recently computed tomography (CT) chest scan and disposable catheter set, physicians are able to navigate to a desired location within the lung to biopsy lesions, stage lymph nodes, insert markers to guide radiotherapy or guide brachytherapy catheters.

Chronic obstructive pulmonary disease (COPD) is a type of obstructive lung disease characterized by long-term breathing problems and poor airflow. The main symptoms include shortness of breath and cough with sputum production. COPD is a progressive disease, meaning it typically worsens over time. Eventually, everyday activities such as walking or getting dressed become difficult. Chronic bronchitis and emphysema are older terms used for different types of COPD. The term "chronic bronchitis" is still used to define a productive cough that is present for at least three months each year for two years. Those with such a cough are at a greater risk of developing COPD. The term "emphysema" is also used for the abnormal presence of air or other gas within tissues.
Physiotherapists treating patients following uncomplicated coronary artery bypass surgery surgery continue to use interventions such as deep breathing exercises that are not supported by best available evidence. Standardised guidelines may be required to better match clinical practice with current literature.
Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH) is a diffuse parenchymal lung disease which often presents with symptoms of cough and shortness of breath. The pathological definition published by the World Health Organization is “a generalized proliferation of scattered single cells, small nodules, or linear proliferations of pulmonary neuroendocrine (PNE) cells that may be confined to the bronchial and bronchiolar epithelium.” The true prevalence of this disease is not known. To date, just under 200 cases have been reported in the literature. However, with an increase in recognition of this disease by radiologists and pulmonologists, the number of cases has been increasing. DIPNECH predominantly affects middle-aged women with slowly progressive lung obstruction. DIPNECH is usually discovered in one of two ways: 1) as an unexpected finding following a lung surgery; or 2) by evaluation of a patient in a pulmonary clinic with longstanding, unexplained symptoms.
Interventional pulmonology is a maturing medical sub-specialty from its parent specialty of pulmonary medicine. It deals specifically with minimally invasive endoscopic and percutaneous procedures for diagnosis and treatment of neoplastic as well as non-neoplastic diseases of the airways, lungs, and pleura. Many IP procedures constitute efficacious yet less invasive alternatives to thoracic surgery.

Balloon pulmonary angioplasty (BPA) is an emerging minimally invasive procedure to treat chronic thromboembolic pulmonary hypertension (CTEPH) in people who are not suitable for pulmonary thromboendarterectomy (PTE) or still have residual pulmonary hypertension and areas of narrowing in the pulmonary arterial tree following previous PTE.
References
- 1 2 Gompelmann D, Eberhardt R, Herth FJ (August 2015). "Novel Endoscopic Approaches to Treating Chronic Obstructive Pulmonary Disease and Emphysema". Seminars in Respiratory and Critical Care Medicine. 36 (4): 609–15. doi:10.1055/s-0035-1555614. PMID 26238645.
- ↑ Belmont, Kristen E. (Nov 1, 2005). "Cholinergic Pathways in the Lungs and Anticholinergic Therapy for Chronic Obstructive Pulmonary Disease". Proceedings of the American Thoracic Society. 2 (4): 297–304. doi:10.1513/pats.200504-043SR. PMID 16267352.