An embolism is the lodging of an embolus, a blockage-causing piece of material, inside a blood vessel. The embolus may be a blood clot (thrombus), a fat globule, a bubble of air or other gas, or foreign material. An embolism can cause partial or total blockage of blood flow in the affected vessel. Such a blockage may affect a part of the body distant to the origin of the embolus. An embolism in which the embolus is a piece of thrombus is called a thromboembolism.

Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.

A thrombus, colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cross-linked fibrin protein. The substance making up a thrombus is sometimes called cruor. A thrombus is a healthy response to injury intended to prevent bleeding, but can be harmful in thrombosis, when clots obstruct blood flow through healthy blood vessels.
Fibrinolysis is a process that prevents blood clots from growing and becoming problematic. This process has two types: primary fibrinolysis and secondary fibrinolysis. The primary type is a normal body process, whereas secondary fibrinolysis is the breakdown of clots due to a medicine, a medical disorder, or some other cause.

Ischemia or ischaemia is a restriction in blood supply to tissues, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue. It also means local anemia in a given part of a body sometimes resulting from constriction. Ischemia comprises not only insufficiency of oxygen, but also reduced availability of nutrients and inadequate removal of metabolic wastes. Ischemia can be partial or total.
Thrombolysis is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and very large pulmonary embolisms.
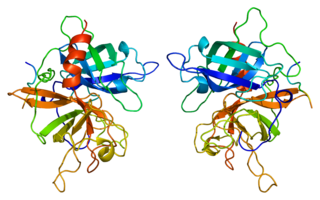
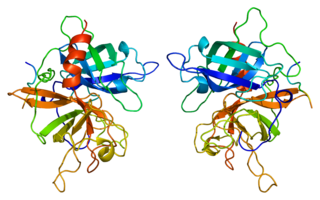
Tissue plasminogen activator is a protein involved in the breakdown of blood clots. It is a serine protease found on endothelial cells, the cells that line the blood vessels. As an enzyme, it catalyzes the conversion of plasminogen to plasmin, the major enzyme responsible for clot breakdown. Human tPA has a molecular weight of ~70 kDa in the single-chain form.
Mechanical thrombectomy, or simply thrombectomy, is the interventional procedure of removing a blood clot (thrombus) from a blood vessel. It is commonly performed in the coronary arteries, peripheral arteries and cerebral arteries.
Alteplase is a thrombolytic drug, used to treat acute myocardial infarctions and other severe conditions caused by blood clotting by breaking up the blood clots that cause them.
Desmoteplase is a novel, highly fibrin-specific "clot-busting" (thrombolytic) drug in development that reached phase III clinical trials. The Danish pharmaceutical company, Lundbeck, owns the worldwide rights to Desmoteplase. In 2009, two large trials were started to test it as a safe and effective treatment for patients with acute ischaemic stroke. After disappointing results in DIAS-3, DIAS-4 was terminated, and in December 2014 Lundbeck announced that they would stop the development of desmoteplase.

A cerebral infarction is an area of necrotic tissue in the brain resulting from a blockage or narrowing in the arteries supplying blood and oxygen to the brain. The restricted oxygen due to the restricted blood supply causes an ischemic stroke that can result in an infarction if the blood flow is not restored within a relatively short period of time. The blockage can be due to a thrombus, an embolus or an atheromatous stenosis of one or more arteries. Which arteries are problematic will determine which areas of the brain are affected (infarcted). These varying infarcts will produce different symptoms and outcomes. About one third will prove fatal.
Ultrasound-enhanced systemic thrombolysis (UEST) is a medical technology that uses ultrasound to enhance the effects of thrombolytic drugs. To treat the blood clots causing strokes, transcranial Doppler ultrasonography is used. It is thought that transcranial doppler ultrasonography aimed at residual obstructive intracranial blood flow may help expose thrombi to tissue plasminogen activator or other thrombolytic drugs.
Embolectomy is the emergency surgical removal of emboli which are blocking blood circulation. It usually involves removal of thrombi, and is then referred to as thrombectomy. Embolectomy is an emergency procedure often as the last resort because permanent occlusion of a significant blood flow to an organ leads to necrosis. Other involved therapeutic options are anticoagulation and thrombolysis.

In medicine, the dense artery sign or hyperdense artery sign is an increased radiodensity of an artery as seen on computer tomography (CT) scans, and is a radiologic sign of early ischemic stroke. In earlier studies of medical imaging in patients with strokes, it was the earliest sign of ischemic stroke in a significant minority of cases. Its appearance portends a poor prognosis for the patient.

Left atrial appendage occlusion (LAAO), also referred to as Left atrial appendage closure (LAAC) is a treatment strategy to reduce the risk of left atrial appendage blood clots from entering the bloodstream and causing a stroke in patients with non-valvular atrial fibrillation (AF).

Acute limb ischaemia (ALI) occurs when there is a sudden lack of blood flow to a limb.

Arterial embolism is a sudden interruption of blood flow to an organ or body part due to an embolus adhering to the wall of an artery blocking the flow of blood, the major type of embolus being a blood clot (thromboembolism). Sometimes, pulmonary embolism is classified as arterial embolism as well, in the sense that the clot follows the pulmonary artery carrying deoxygenated blood away from the heart. However, pulmonary embolism is generally classified as a form of venous embolism, because the embolus forms in veins. Arterial embolism is the major cause of infarction.

Darexaban (YM150) is a direct inhibitor of factor Xa created by Astellas Pharma. It is an experimental drug that acts as an anticoagulant and antithrombotic to prevent venous thromboembolism after a major orthopaedic surgery, stroke in patients with atrial fibrillation and possibly ischemic events in acute coronary syndrome. It is used in form of the maleate. The development of darexaban was discontinued in September 2011.

Perfusion MRI or perfusion-weighted imaging (PWI) is perfusion scanning by the use of a particular MRI sequence. The acquired data are then postprocessed to obtain perfusion maps with different parameters, such as BV, BF, MTT and TTP.