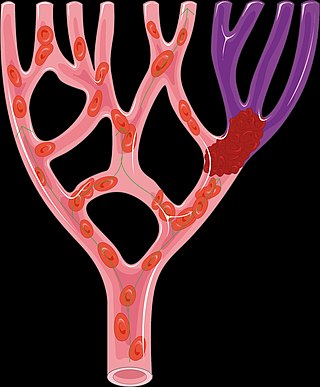
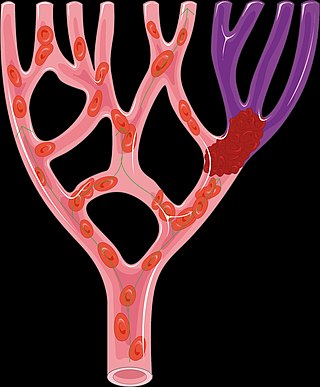
An embolism is the lodging of an embolus, a blockage-causing piece of material, inside a blood vessel. The embolus may be a blood clot (thrombus), a fat globule, a bubble of air or other gas, amniotic fluid, or foreign material.

Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.

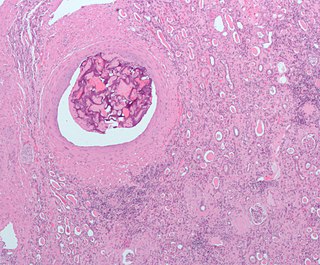
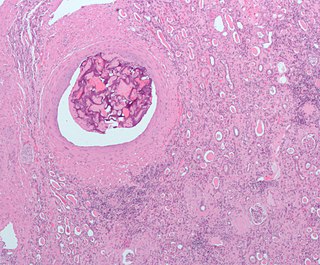
A thrombus, colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cross-linked fibrin protein. The substance making up a thrombus is sometimes called cruor. A thrombus is a healthy response to injury intended to stop and prevent further bleeding, but can be harmful in thrombosis, when a clot obstructs blood flow through healthy blood vessels in the circulatory system.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction.

Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.

Thromboembolism is a condition in which a blood clot (thrombus) breaks off from its original site and travels through the bloodstream to obstruct a blood vessel, causing tissue ischemia and organ damage. Thromboembolism can affect both the venous and arterial systems, with different clinical manifestations and management strategies.
Mechanical thrombectomy, or simply thrombectomy, is the removal of a blood clot (thrombus) from a blood vessel, often and especially endovascularly as an interventional radiology procedure called endovascular thrombectomy (EVT). It thus contrasts with thrombolysis by thrombolytic medications, as either alternative or complement thereto. It is commonly performed in the cerebral arteries as treatment to reverse the ischemia in some ischemic strokes. Open vascular surgery versions of thrombectomy also exist. The effectiveness of thrombectomy for strokes was confirmed in several randomised clinical trials conducted at various medical centers throughout the United States, as reported in a seminal multistudy report in 2015.
Alteplase, sold under the brand name Activase among others, is a biosynthetic form of human tissue-type plasminogen activator (t-PA). It is a thrombolytic medication used to treat acute ischemic stroke, acute ST-elevation myocardial infarction, pulmonary embolism associated with low blood pressure, and blocked central venous catheter. It is given by injection into a vein or artery. Alteplase is the same as the normal human plasminogen activator produced in vascular endothelial cells and is synthesized via recombinant DNA technology in Chinese hamster ovary cells (CHO). Alteplase causes the breakdown of a clot by inducing fibrinolysis.

Cerebral infarction is the pathologic process that results in an area of necrotic tissue in the brain. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia), most commonly due to thromboembolism, and manifests clinically as ischemic stroke. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.
An embolus, is described as a free-floating mass, located inside blood vessels that can travel from one site in the blood stream to another. An embolus can be made up of solid, liquid, or gas. Once these masses get "stuck" in a different blood vessel, it is then known as an "embolism." An embolism can cause ischemia—damage to an organ from lack of oxygen. A paradoxical embolism is a specific type of embolism in which the embolus travels from the right side of the heart to the left side of the heart and lodges itself in a blood vessel known as an artery. Thus, it is termed "paradoxical" because the embolus lands in an artery, rather than a vein.

A watershed stroke is defined as a brain ischemia that is localized to the vulnerable border zones between the tissues supplied by the anterior, posterior and middle cerebral arteries. The actual blood stream blockage/restriction site can be located far away from the infarcts. Watershed locations are those border-zone regions in the brain supplied by the major cerebral arteries where blood supply is decreased. Watershed strokes are a concern because they comprise approximately 10% of all ischemic stroke cases. The watershed zones themselves are particularly susceptible to infarction from global ischemia as the distal nature of the vasculature predisposes these areas to be most sensitive to profound hypoperfusion.

In thoracic surgery, a pulmonary thromboendarterectomy (PTE), also referred to as pulmonary endarterectomy (PEA), is an operation that removes organized clotted blood (thrombus) from the pulmonary arteries, which supply blood to the lungs.

Acute limb ischaemia (ALI) occurs when there is a sudden lack of blood flow to a limb, within 14 days of symptoms onset. It is different from another condition which is more chronic called critical limb ischemia (CLD). CLD is the end stage of peripheral vascular disease where there is still some collateral circulation (alternate circulation pathways} that bring some blood to the distal parts of the limbs. While limbs in both acute and chronic limb ischemia may be pulseless, a chronically ischemic limb is typically warm and pink due to a well-developed collateral artery network and does not need emergency intervention to avoid limb loss.

Arterial embolism is a sudden interruption of blood flow to an organ or body part due to an embolus adhering to the wall of an artery blocking the flow of blood, the major type of embolus being a blood clot (thromboembolism). Sometimes, pulmonary embolism is classified as arterial embolism as well, in the sense that the clot follows the pulmonary artery carrying deoxygenated blood away from the heart. However, pulmonary embolism is generally classified as a form of venous embolism, because the embolus forms in veins. Arterial embolism is the major cause of infarction.

A limb infarction is an area of tissue death of an arm or leg. It may cause skeletal muscle infarction, avascular necrosis of bones, or necrosis of a part of or an entire limb.
Blood clots are a relatively common occurrence in the general population and are seen in approximately 1-2% of the population by age 60. Typically, blood clots develop in the deep veins of the lower extremities, deep vein thrombosis (DVT) or as a blood clot in the lung, pulmonary embolism. A very small number of people who develop blood clots have a more serious and often life-threatening condition, known as thrombotic storm (TS). TS is characterized by the development of more than one blood clot in a short period of time. These clots often occur in multiple and sometimes unusual locations in the body and are often difficult to treat. TS may be associated with an existing condition or situation that predisposes a person to blood clots, such as injury, infection, or pregnancy. In many cases, a risk assessment will identify interventions that will prevent the formation of blood clots.

Arterial occlusion is a condition involving partial or complete blockage of blood flow through an artery. Arteries are blood vessels that carry oxygenated blood to body tissues. An occlusion of arteries disrupts oxygen and blood supply to tissues, leading to ischemia. Depending on the extent of ischemia, symptoms of arterial occlusion range from simple soreness and pain that can be relieved with rest, to a lack of sensation or paralysis that could require amputation.

Feline arterial thromboembolism is a disease of the domestic cat in which blood clots (thrombi) block arteries, causing severe circulatory problems. Relative to the total number of feline patients, the disease is rare, but relatively common in cats with heart disease: about one-sixth of cats with heart disease are affected. Heart disease is the most common underlying cause of arterial thromboembolism. It leads to the formation of blood clots in the heart, which leave it with the bloodstream and obstruct larger blood vessels, in cats mainly the aorta at the outlet of the two external iliac arteries. Arterial thromboembolism occurs suddenly and is very painful. The blockage of the terminal portion of the aorta results in an undersupply of blood to the hind legs. The result is paralysis, cold hind extremities and later severe tissue damage. Rarely, other blood vessels are also affected; the symptoms of failure then depend on the supply area of the affected artery. Since drug thrombolysis in cats does not achieve satisfactory results, the focus today is on the self-dissolution of the clot by the body's own repair processes. Accompanying pain therapy and thrombosis prevention are performed and the underlying disease is treated. The mortality of arterial thromboembolism in cats is very high. Fifty to 60% of affected animals are euthanized without attempted treatment, and only one-quarter to one-third of animals survive such an event. In about half of the recovered cats, thromboembolism recurs despite anticoagulation prophylaxis.