Workflow

Validation and verification are procedures that ensure that medical devices fulfil their intended purpose. Validation or verification is generally needed when a health facility acquires a new device to perform medical tests.
The main difference between the two is that validation is focused on ensuring that the device meets the needs and requirements of its intended users and the intended use environment, whereas verification is focused on ensuring that the device meets its specified design requirements.
For instance, a regulatory agency (such as CE or FDA) may ensure that a product has been validated for general use before approval. An individual laboratory that introduces such an approved medical device may then not need to perform their own validation, but generally still need to perform verification to ensure that the device works correctly. [1]

Standards for validation and verification of medical laboratories are outlined in the international standard ISO 15189, in addition to national and regional regulations. [1]
As per United States federal regulations, the following analytical tests need to be done by a medical laboratory that introduces a new testing device:
| Parameter(s) | Verification of FDA-approved device | Validation of a laboratory-developed test |
|---|---|---|
| Accuracy and precision | Yes [2] [3] | Yes [2] [3] |
| Reportable range | Yes [2] [3] | Yes [2] [3] |
| Analytical sensitivity | Yes [2] | Yes [2] [3] |
| Analytical specificity | Yes [2] [3] | |
| Reference range | Verification [2] | Establishment [2] |
| Carryover effect | Yes [2] | |
| Sample/materials stability | Yes [2] |
To establish a reference range, the Clinical and Laboratory Standards Institute (CLSI) recommends testing at least 120 patient samples. In contrast, for the verification of a reference range, it is recommended to use a total of 40 samples, 20 from healthy men and 20 from healthy women, and the results should be compared to the published reference range. The results should be evenly spread throughout the published reference range rather than clustered at one end. The published reference range can be accepted for use if 95% of the results fall within it. Otherwise, the laboratory needs to establish its own reference range. [4]

Hazard analysis and critical control points, or HACCP, is a systematic preventive approach to food safety from biological, chemical, and physical hazards in production processes that can cause the finished product to be unsafe and designs measures to reduce these risks to a safe level. In this manner, HACCP attempts to avoid hazards rather than attempting to inspect finished products for the effects of those hazards. The HACCP system can be used at all stages of a food chain, from food production and preparation processes including packaging, distribution, etc. The Food and Drug Administration (FDA) and the United States Department of Agriculture (USDA) require mandatory HACCP programs for juice and meat as an effective approach to food safety and protecting public health. Meat HACCP systems are regulated by the USDA, while seafood and juice are regulated by the FDA. All other food companies in the United States that are required to register with the FDA under the Public Health Security and Bioterrorism Preparedness and Response Act of 2002, as well as firms outside the US that export food to the US, are transitioning to mandatory hazard analysis and risk-based preventive controls (HARPC) plans.

Current good manufacturing practices (cGMP) are those conforming to the guidelines recommended by relevant agencies. Those agencies control the authorization and licensing of the manufacture and sale of food and beverages, cosmetics, pharmaceutical products, dietary supplements, and medical devices. These guidelines provide minimum requirements that a manufacturer must meet to assure that their products are consistently high in quality, from batch to batch, for their intended use. The rules that govern each industry may differ significantly; however, the main purpose of GMP is always to prevent harm from occurring to the end user. Additional tenets include ensuring the end product is free from contamination, that it is consistent in its manufacture, that its manufacture has been well documented, that personnel are well trained, and that the product has been checked for quality more than just at the end phase. GMP is typically ensured through the effective use of a quality management system (QMS).
A medical device is any device intended to be used for medical purposes. Significant potential for hazards are inherent when using a device for medical purposes and thus medical devices must be proved safe and effective with reasonable assurance before regulating governments allow marketing of the device in their country. As a general rule, as the associated risk of the device increases the amount of testing required to establish safety and efficacy also increases. Further, as associated risk increases the potential benefit to the patient must also increase.
An electronic lab notebook is a computer program designed to replace paper laboratory notebooks. Lab notebooks in general are used by scientists, engineers, and technicians to document research, experiments, and procedures performed in a laboratory. A lab notebook is often maintained to be a legal document and may be used in a court of law as evidence. Similar to an inventor's notebook, the lab notebook is also often referred to in patent prosecution and intellectual property litigation.
Software assurance (SwA) is a critical process in software development that ensures the reliability, safety, and security of software products. It involves a variety of activities, including requirements analysis, design reviews, code inspections, testing, and formal verification. One crucial component of software assurance is secure coding practices, which follow industry-accepted standards and best practices, such as those outlined by the Software Engineering Institute (SEI) in their CERT Secure Coding Standards (SCS).
In the experimental (non-clinical) research arena, good laboratory practice or GLP is a quality system of management controls for research laboratories and organizations to ensure the uniformity, consistency, reliability, reproducibility, quality, and integrity of products in development for human or animal health through non-clinical safety tests; from physio-chemical properties through acute to chronic toxicity tests.
The process of establishing documentary evidence demonstrating that a procedure, process, or activity carried out in testing and then production maintains the desired level of compliance at all stages. In the pharmaceutical industry, it is very important that in addition to final testing and compliance of products, it is also assured that the process will consistently produce the expected results. The desired results are established in terms of specifications for outcome of the process. Qualification of systems and equipment is therefore a part of the process of validation. Validation is a requirement of food, drug and pharmaceutical regulating agencies such as the US FDA and their good manufacturing practices guidelines. Since a wide variety of procedures, processes, and activities need to be validated, the field of validation is divided into a number of subsections including the following:
ISO 15189 Medical laboratories — Requirements for quality and competence is an international standard that specifies the quality management system requirements particular to medical laboratories. The standard was developed by the International Organisation for Standardization's Technical Committee 212. ISO/TC 212 assigned ISO 15189 to a working group to prepare the standard based on the details of ISO/IEC 17025:1999 General requirements for the competence of testing and calibration laboratories. This working group included provision of advice to medical laboratory users, including specifics on the collection of patient samples, the interpretation of test results, acceptable turnaround times, how testing is to be provided in a medical emergency, and the lab's role in the education and training of health care staff. While the standard is based on ISO/IEC 17025 and ISO 9001, it is a unique document that takes into consideration the specific requirements of the medical environment and the importance of the medical laboratory to patient care.
A design history file is a compilation of documentation that describes the design history of a finished medical device. The design history file, or DHF, is part of regulation introduced in 1990 when the U.S. Congress passed the Safe Medical Devices Act, which established new standards for medical devices that can cause or contribute to the death, serious illness, or injury of a patient. Prior to this legislation, U.S. Food and Drug Administration (FDA) auditors were limited to examining the production and quality control records of the device.
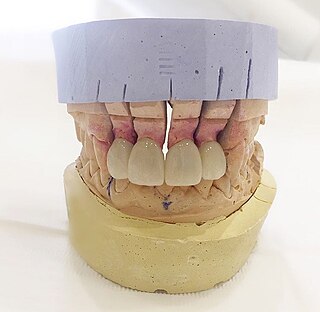
Dental laboratories manufacture or customize a variety of products to assist in the provision of oral health care by a licensed dentist. These products include crowns, bridges, dentures and other dental products. Dental lab technicians follow a prescription from a licensed dentist when manufacturing these items, which include prosthetic devices and therapeutic devices. The FDA regulates these products as medical devices and they are therefore subject to FDA's good manufacturing practice ("GMP") and quality system ("QS") requirements. In most cases, however, they are exempt from manufacturer registration requirements. Some of the most common restorations manufactured include crowns, bridges, dentures, and dental implants. Dental implants is one of the most advanced dental technologies in the field of dentistry.
Public health laboratories (PHLs) are governmental reference laboratories that protect the public against diseases and other health hazards. The 2005 International Health Regulations came into force in June 2007, with 196 binding countries that recognised that certain public health incidents, extending beyond disease, ought to be designated as a Public Health Emergency of International Concern (PHEIC), as they pose a significant global threat. The PHLs serve as national hazard detection centres, and forward these concerns to the World Health Organization.
In natural and social science research, a protocol is most commonly a predefined procedural method in the design and implementation of an experiment. Protocols are written whenever it is desirable to standardize a laboratory method to ensure successful replication of results by others in the same laboratory or by other laboratories. Additionally, and by extension, protocols have the advantage of facilitating the assessment of experimental results through peer review. In addition to detailed procedures, equipment, and instruments, protocols will also contain study objectives, reasoning for experimental design, reasoning for chosen sample sizes, safety precautions, and how results were calculated and reported, including statistical analysis and any rules for predefining and documenting excluded data to avoid bias.
The South African National Accreditation System (SANAS) is the official accreditation body for South Africa. Founded in 1996, SANAS is headquartered in Pretoria, South Africa. SANAS accreditation certificates are a formal recognition by the Government of South Africa that an organisation is competent to perform specific tasks.

A medical laboratory or clinical laboratory is a laboratory where tests are conducted out on clinical specimens to obtain information about the health of a patient to aid in diagnosis, treatment, and prevention of disease. Clinical medical laboratories are an example of applied science, as opposed to research laboratories that focus on basic science, such as found in some academic institutions.
Verification and validation are independent procedures that are used together for checking that a product, service, or system meets requirements and specifications and that it fulfills its intended purpose. These are critical components of a quality management system such as ISO 9000. The words "verification" and "validation" are sometimes preceded with "independent", indicating that the verification and validation is to be performed by a disinterested third party. "Integration verification and validation" can be abbreviated as "IV&V".
The College of American Pathologists (CAP) is a member-based physician organization founded in 1946 comprising approximately 18,000 board-certified pathologists. It serves patients, pathologists, and the public by fostering and advocating best practices in pathology and laboratory medicine.
Laboratory quality control is designed to detect, reduce, and correct deficiencies in a laboratory's internal analytical process prior to the release of patient results, in order to improve the quality of the results reported by the laboratory. Quality control (QC) is a measure of precision, or how well the measurement system reproduces the same result over time and under varying operating conditions. Laboratory quality control material is usually run at the beginning of each shift, after an instrument is serviced, when reagent lots are changed, after equipment calibration, and whenever patient results seem inappropriate. Quality control material should approximate the same matrix as patient specimens, taking into account properties such as viscosity, turbidity, composition, and color. It should be simple to use, with minimal vial-to-vial variability, because variability could be misinterpreted as systematic error in the method or instrument. It should be stable for long periods of time, and available in large enough quantities for a single batch to last at least one year. Liquid controls are more convenient than lyophilized (freeze-dried) controls because they do not have to be reconstituted, minimizing pipetting error. Dried Tube Specimen (DTS) is slightly cumbersome as a QC material but it is very low-cost, stable over long periods and efficient, especially useful for resource-restricted settings in under-developed and developing countries. DTS can be manufactured in-house by a laboratory or Blood Bank for its use.
Design controls designates the application of a formal methodology to the conduct of product development activities. It is often mandatory to implement such practice when designing and developing products within regulated industries.
A First Article Inspection (FAI) is a production validation process for verifying that a new or modified production process produces conforming parts that meet the manufacturing specification detailed in technical or engineering drawings. Typically, a supplier performs the FAI and the purchaser reviews the report. The FAI process usually consists of fully testing and inspecting either the first part produced by the new process or a sample from the first batch of parts. First article inspection is typically a purchase order requirement of the purchaser for the supplier to complete. If the manufacturer doesn't have the in-house capability or if the purchaser requests, the first article inspection may be conducted by an approved subcontract supplier such as a dimensional inspection/metrology laboratory.

Package testing or packaging testing involves the measurement of a characteristic or property involved with packaging. This includes packaging materials, packaging components, primary packages, shipping containers, and unit loads, as well as the associated processes.
{{cite journal}}: CS1 maint: multiple names: authors list (link)