Related Research Articles
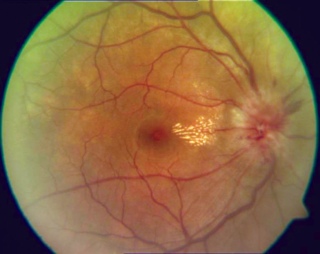
Optic neuritis describes any condition that causes inflammation of the optic nerve; it may be associated with demyelinating diseases, or infectious or inflammatory processes.

Transverse myelitis (TM) is a rare neurological condition wherein the spinal cord is inflamed. The adjective transverse implies that the spinal inflammation (myelitis) extends horizontally throughout the cross section of the spinal cord; the terms partial transverse myelitis and partial myelitis are sometimes used to specify inflammation that affects only part of the width of the spinal cord. TM is characterized by weakness and numbness of the limbs, deficits in sensation and motor skills, dysfunctional urethral and anal sphincter activities, and dysfunction of the autonomic nervous system that can lead to episodes of high blood pressure. Signs and symptoms vary according to the affected level of the spinal cord. The underlying cause of TM is unknown. The spinal cord inflammation seen in TM has been associated with various infections, immune system disorders, or damage to nerve fibers, by loss of myelin. As opposed to leukomyelitis which affects only the white matter, it affects the entire cross-section of the spinal cord. Decreased electrical conductivity in the nervous system can result.

Tetraplegia, also known as quadriplegia, is defined as the dysfunction or loss of motor and/or sensory function in the cervical area of the spinal cord. A loss of motor function can present as either weakness or paralysis leading to partial or total loss of function in the arms, legs, trunk, and pelvis; paraplegia is similar but affects the thoracic, lumbar, and sacral segments of the spinal cord and arm function is spared. The paralysis may be flaccid or spastic. A loss of sensory function can present as an impairment or complete inability to sense light touch, pressure, heat, pinprick/pain, and proprioception. In these types of spinal cord injury, it is common to have a loss of both sensation and motor control.

The radial nerve is a nerve in the human body that supplies the posterior portion of the upper limb. It innervates the medial and lateral heads of the triceps brachii muscle of the arm, as well as all 12 muscles in the posterior osteofascial compartment of the forearm and the associated joints and overlying skin.
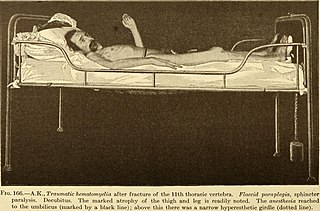
Paraplegia, or paraparesis, is an impairment in motor or sensory function of the lower extremities. The word comes from Ionic Greek (παραπληγίη) "half-stricken". It is usually caused by spinal cord injury or a congenital condition that affects the neural (brain) elements of the spinal canal. The area of the spinal canal that is affected in paraplegia is either the thoracic, lumbar, or sacral regions. If four limbs are affected by paralysis, tetraplegia or quadriplegia is the correct term. If only one limb is affected, the correct term is monoplegia. Spastic paraplegia is a form of paraplegia defined by spasticity of the affected muscles, rather than flaccid paralysis.

The vestibular system, in vertebrates, is a sensory system that creates the sense of balance and spatial orientation for the purpose of coordinating movement with balance. Together with the cochlea, a part of the auditory system, it constitutes the labyrinth of the inner ear in most mammals.

Peripheral neuropathy, often shortened to neuropathy, is a general term describing damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland, or organ function depending on which nerves are affected; in other words, neuropathy affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.
Robert Wartenberg was a clinical neurologist and professor.

Sensory neurons, also known as afferent neurons, are neurons in the nervous system, that convert a specific type of stimulus, via their receptors, into action potentials or graded potentials. This process is called sensory transduction. The cell bodies of the sensory neurons are located in the dorsal ganglia of the spinal cord.

Labyrinthitis is inflammation of the labyrinth, a maze of fluid-filled channels in the inner ear. Vestibular neuritis is inflammation of the vestibular nerve. Both conditions involve inflammation of the inner ear. Labyrinths that house the vestibular system sense changes in the head's position or the head's motion. Inflammation of these inner ear parts results in a sensation of the world spinning and also possible hearing loss or ringing in the ears. It can occur as a single attack, a series of attacks, or a persistent condition that diminishes over three to six weeks. It may be associated with nausea, vomiting, and eye nystagmus.

Neuritis is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
Monoplegia is paralysis of a single limb, usually an arm. Common symptoms associated with monoplegic patients are weakness, numbness, and pain in the affected limb. Monoplegia is a type of paralysis that falls under hemiplegia. While hemiplegia is paralysis of half of the body, monoplegia is localized to a single limb or to a specific region of the body. Monoplegia of the upper limb is sometimes referred to as brachial monoplegia, and that of the lower limb is called crural monoplegia. Monoplegia in the lower extremities is not as common of an occurrence as in the upper extremities. Monoparesis is a similar, but less severe, condition because one limb is very weak, not paralyzed. For more information, see paresis.
In physiology, motor coordination is the orchestrated movement of multiple body parts as required to accomplish intended actions, like walking. This coordination is achieved by adjusting kinematic and kinetic parameters associated with each body part involved in the intended movement. The modifications of these parameters typically relies on sensory feedback from one or more sensory modalities, such as proprioception and vision.

Photopsia is the presence of perceived flashes of light in the field of vision.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
Anterior interosseous syndrome is a medical condition in which damage to the anterior interosseous nerve (AIN), a distal motor and sensory branch of the median nerve, classically with severe weakness of the pincer movement of the thumb and index finger, and can cause transient pain in the wrist.

Proprioception, also called kinaesthesia, is the sense of self-movement, force, and body position. It is sometimes described as the "sixth sense".
A somatosensory disorder is an impairment of the somatosensory system.

Allochiria is a neurological disorder in which the patient responds to stimuli presented to one side of their body as if the stimuli had been presented at the opposite side. It is associated with spatial transpositions, usually symmetrical, of stimuli from one side of the body to the opposite one. Thus a touch to the left side of the body will be reported as a touch to the right side, which is also known as somatosensory allochiria. If the auditory or visual senses are affected, sounds will be reported as being heard on the opposite side to that on which they occur and objects presented visually will be reported as having been presented on the opposite side. Often patients may express allochiria in their drawing while copying an image. Allochiria often co-occurs with unilateral neglect and, like hemispatial neglect, the disorder arises commonly from damage to the right parietal lobe.

Cheiralgia paraesthetica is a neuropathy of the hand generally caused by compression or trauma to the superficial branch of the radial nerve. The area affected is typically on the back or side of the hand at the base of the thumb, near the anatomical snuffbox, but may extend up the back of the thumb and index finger and across the back of the hand. Symptoms include numbness, tingling, burning or pain. Since the nerve branch is sensory there is no motor impairment. It may be distinguished from de Quervain syndrome because it is not dependent on motion of the hand or fingers.
References
- ↑ Katirji, Bashar; Kaminski, Henry J.; Ruff, Robert L. (2013). Neuromuscular Disorders in Clinical Practice. Springer Science & Business Media. p. 743. ISBN 9781461465676.
- ↑ Matthews WB, Esiri M (1983). "The migrant sensory neuritis of Wartenberg". Journal of Neurology, Neurosurgery & Psychiatry. 46 (1): 1–4. doi:10.1136/jnnp.46.1.1. PMC 1027254 . PMID 6842194.