Related Research Articles

HIV/AIDS originated in the early 20th century and has become a major public health concern and cause of death in many countries. AIDS rates varies significantly between countries, with the majority of cases concentrated in Southern Africa. Although the continent is home to about 15.2 percent of the world's population, more than two-thirds of the total population infected worldwide – approximately 35 million people – were Africans, of whom around 1 million have already died. Eastern and Southern Africa alone accounted for an estimate of 60 percent of all people living with HIV and 100 percent of all AIDS deaths in 2011. The countries of Eastern and Southern Africa are most affected, leading to raised death rates and lowered life expectancy among adults between the ages of 20 and 49 by about twenty years. Furthermore, life expectancy in many parts of Africa is declining, largely as a result of the HIV/AIDS epidemic, with life-expectancy in some countries reaching as low as thirty-nine years.

The global pandemic of HIV/AIDS began in 1981, and is an ongoing worldwide public health issue. According to the World Health Organization (WHO), by 2023, HIV/AIDS had killed approximately 40.4 million people, and approximately 39 million people were infected with HIV globally. Of these, 29.8 million people (75%) are receiving antiretroviral treatment. There were about 630,000 deaths from HIV/AIDS in 2022. The 2015 Global Burden of Disease Study estimated that the global incidence of HIV infection peaked in 1997 at 3.3 million per year. Global incidence fell rapidly from 1997 to 2005, to about 2.6 million per year. Incidence of HIV has continued to fall, decreasing by 23% from 2010 to 2020, with progress dominated by decreases in Eastern Africa and Southern Africa. As of 2020, there are approximately 1.5 million new infections of HIV per year globally.

HIV/AIDS in India is an epidemic. The National AIDS Control Organisation (NACO) estimated that 3.14 million people lived with HIV/AIDS in India in 2023. Despite being home to the world's third-largest population of persons with HIV/AIDS, the AIDS prevalence rate in India is lower than that of many other countries. In 2016, India's AIDS prevalence rate stood at approximately 0.30%—the 80th highest in the world. Treatment of HIV/AIDS is via a combination of antiretroviral drugs and education programs to help people avoid infection.

Taiwan's epidemic of HIV/AIDS began with the first case reported in December 1984. On 17 December 1990 the government promulgated the AIDS Prevention and Control Act. On 11 July 2007, the AIDS Prevention and Control Act was renamed the HIV Infection Control and Patient Rights Protection Act.
The Caribbean is the second-most affected region in the world in terms of HIV prevalence rates. Based on 2009 data, about 1.0 percent of the adult population is living with the disease, which is higher than any other region except Sub-Saharan Africa. Several factors influence this epidemic, including poverty, gender, sex tourism, and stigma. HIV incidence in the Caribbean declined 49% between 2001 and 2012. Different countries have employed a variety of responses to the disease, with a range of challenges and successes.

HIV/AIDS is one of the most serious health concerns in South Africa. The country has the highest number of people afflicted with HIV of any country, and the fourth-highest adult HIV prevalence rate, according to the 2019 United Nations statistics.
Beatrice Were is a Ugandan AIDS activist.
The history of HIV/AIDS in Australia is distinctive, as Australian government bodies recognised and responded to the AIDS pandemic relatively swiftly, with the implementation of effective disease prevention and public health programs, such as needle and syringe programs (NSPs). As a result, despite significant numbers of at-risk group members contracting the virus in the early period following its discovery, Australia achieved and has maintained a low rate of HIV infection in comparison to the rest of the world.
Youthforce was an international youth network founded in 1999 to raise visibility around the impact of HIV/AIDS on youth.

Although almost no research existed on the role of women in Angolan society in the late 1980s, there are a few generalities that could be drawn. In rural Angola, as in many African economies, most of the population engaged in agricultural activities. Women performed much of the agricultural labor. Marriage generally involved familial, political, and economic interests as well as personal considerations and gains. The household was the most important unit of production and was usually composed of several generations. The women grew and prepared most of the food for the household and performed all other domestic work. Because of their major role in food production, women shared relatively equal status with men, who spent much of their time hunting or tending cattle.

Bisi Alimi is a British-Nigerian gay rights activist, public speaker, blog writer and HIV/LGBT advocate who gained international attention when he became the first Nigerian to come out on television.
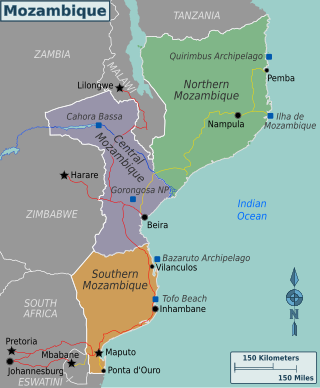
Mozambique is a country particularly hard-hit by the HIV/AIDS epidemic. According to 2008 UNAIDS estimates, this southeast African nation has the 8th highest HIV rate in the world. With 1,600,000 Mozambicans living with HIV, 990,000 of which are women and children, Mozambique's government realizes that much work must be done to eradicate this infectious disease. To reduce HIV/AIDS within the country, Mozambique has partnered with numerous global organizations to provide its citizens with augmented access to antiretroviral therapy and prevention techniques, such as condom use. A surge toward the treatment and prevention of HIV/AIDS in women and children has additionally aided in Mozambique's aim to fulfill its Millennium Development Goals (MDGs). Nevertheless, HIV/AIDS has made a drastic impact on Mozambique; individual risk behaviors are still greatly influenced by social norms, and much still needs to be done to address the epidemic and provide care and treatment to those in need.

HIV/AIDS in Nigeria was a concern in the 2000s, when an estimated seven million people had HIV/AIDS. In 2008, the HIV prevalence rate among adults aged between 15 and 49 was 3.9 percent, in 2018 the rate among adults aged between 15 and 65 was 1.5 percent. As elsewhere in Africa, women are statistically more likely to have HIV/AIDS. The Nigeria HIV/AIDS Indicator and Impact Survey was the world's largest and presented statistics which showed the overall numbers were lower than expected. Antiretroviral treatment is available, but people prefer to take the therapy secretly, since there is still noticeable discrimination against people with HIV/AIDS.
There is a relatively low prevalence of HIV/AIDS in New Zealand, with an estimated 2,900 people out a population of 4.51 million living with HIV/AIDS as of 2014. The rate of newly diagnosed HIV infections was stable at around 100 annually through the late 1980s and the 1990s but rose sharply from 2000 to 2005. It has since stabilised at roughly 200 new cases annually. Male-to-male sexual contact has been the largest contributor to new HIV cases in New Zealand since record began in 1985. Heterosexual contact is the second largest contributor to new cases, but unlike male-to-male contact, they are mostly acquired outside New Zealand. In 2018 the New Zealand Government reported a “major reduction” in the number of people diagnosed with HIV.

Reverend Canon Gideon Byamugisha is an Anglican priest in Uganda with a parish outside of Kampala. In 1992, he became the first religious leader in Africa to publicly announce that he was HIV positive. In 2009, Byamugisha received the 26th annual Niwano Peace Prize "in recognition of his work to uphold the dignity and human rights of people living with HIV/AIDS".
The relationship between religion and HIV/AIDS has been an ongoing one, since the advent of the pandemic. Many faith communities have participated in raising awareness about HIV/AIDS, offering free treatment, as well as promoting HIV/AIDS testing and preventative measures. Christian denominations, such as Lutheranism and Methodism, have advocated for the observance of World AIDS Day to educate their congregations about the disease. Some Churches run voluntary blood testing camps and counselling centers to diagnose and help those affected by HIV/AIDS.
Discrimination against people with HIV/AIDS or serophobia is the prejudice, fear, rejection, and stigmatization of people with HIV/AIDS. Marginalized, at-risk groups such as members of the LGBTQ+ community, intravenous drug users, and sex workers are most vulnerable to facing HIV/AIDS discrimination. The consequences of societal stigma against PLHIV are quite severe, as HIV/AIDS discrimination actively hinders access to HIV/AIDS screening and care around the world. Moreover, these negative stigmas become used against members of the LGBTQ+ community in the form of stereotypes held by physicians.
Initial events and trends in the discussion of HIV and AIDS in mass media contributed to the stigma and discrimination against those affected with the disease. Later discussion, sometimes led by HIV+ individuals themselves, moved toward advocacy and education on disease prevention and management. The UNESCO report on Journalism Education says, "Well researched television content can create public awareness about HIV prevention, treatment, care and support can potentially influence the development and implementation of relevant policies."

South Africa's HIV/AIDS epidemic, which is among the most severe in the world, is concentrated in its townships, where many black South Africans live due to the lingering effects of the Group Areas Act.
Jẹ́gẹ́dẹ́ is a Yoruba male given name or family name. Notable people with the name include:
References
- ↑ "Positive mother speaks out". The New Humanitarian. 27 April 2007. Retrieved June 3, 2020.
- 1 2 3 "Positive mother speaks out". The New Humanitarian. United Nations Office for the Coordination of Humanitarian Affairs. 25 April 2007. Retrieved 5 May 2020.
- 1 2 3 Donnelly, John (10 March 2004). "A name, not a number - Taipei Times". Taipei Times. Archived from the original on 1 September 2006. Retrieved 5 May 2020.
- 1 2 Fleshman, Michael. "Women: the face of AIDS in Africa". Africa Renewal. United Nations Department of Public Information. Archived from the original on 1 May 2019. Retrieved 5 May 2020.
- 1 2 Cunningham, Carissa (18 March 2004). "Human rights award winner speaks at SPH". Harvard Gazette. Retrieved 5 May 2020.
- ↑ Staff, W. W. D. (7 May 2004). "Reebok's Human Rights Stars". WWD. Retrieved 5 May 2020.