Related Research Articles
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.
The spread of HIV/AIDS has affected millions of people worldwide; AIDS is considered a pandemic. The World Health Organization (WHO) estimated that in 2016 there were 36.7 million people worldwide living with HIV/AIDS, with 1.8 million new HIV infections per year and 1 million deaths due to AIDS. Misconceptions about HIV and AIDS arise from several different sources, from simple ignorance and misunderstandings about scientific knowledge regarding HIV infections and the cause of AIDS to misinformation propagated by individuals and groups with ideological stances that deny a causative relationship between HIV infection and the development of AIDS. Below is a list and explanations of some common misconceptions and their rebuttals.

The global epidemic of HIV/AIDS began in 1981, and is an ongoing worldwide public health issue. According to the World Health Organization (WHO), as of 2021, HIV/AIDS has killed approximately 40.1 million people, and approximately 38.4 million people are infected with HIV globally. Of these 38.4 million people, 75% are receiving antiretroviral treatment. There were about 770,000 deaths from HIV/AIDS in 2018, and 650,000 deaths in 2021. The 2015 Global Burden of Disease Study estimated that the global incidence of HIV infection peaked in 1997 at 3.3 million per year. Global incidence fell rapidly from 1997 to 2005, to about 2.6 million per year. Incidence of HIV has continued to fall, decreasing by 23% from 2010 to 2020, with progress dominated by decreases in Eastern Africa and Southern Africa. As of 2020, there are approximately 1.5 million new infections of HIV per year globally.

Human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), a retrovirus. Following initial infection an individual may not notice any symptoms, or may experience a brief period of influenza-like illness. Typically, this is followed by a prolonged incubation period with no symptoms. If the infection progresses, it interferes more with the immune system, increasing the risk of developing common infections such as tuberculosis, as well as other opportunistic infections, and tumors which are rare in people who have normal immune function. These late symptoms of infection are referred to as acquired immunodeficiency syndrome (AIDS). This stage is often also associated with unintended weight loss.

Taiwan's epidemic of HIV/AIDS began with the first case reported in December 1984. On 17 December 1990 the government promulgated the AIDS Prevention and Control Act. On 11 July 2007, the AIDS Prevention and Control Act was renamed the HIV Infection Control and Patient Rights Protection Act.
Human Immunodeficiency Virus (HIV) and Hepatitis C Virus (HCV) co-infection is a multi-faceted, chronic condition that significantly impacts public health. According to the World Health Organization (WHO), 2 to 15% of those infected with HIV are also affected by HCV, increasing their risk of morbidity and mortality due to accelerated liver disease. The burden of co-infection is especially high in certain high-risk groups, such as intravenous drug users and men who have sex with men. These individuals who are HIV-positive are commonly co-infected with HCV due to shared routes of transmission including, but not limited to, exposure to HIV-positive blood, sexual intercourse, and passage of the Hepatitis C virus from mother to infant during childbirth.

In Western Europe, the routes of transmission of HIV are diverse, including paid sex, sex between men, intravenous drugs, mother to child transmission, and heterosexual sex. However, many new infections in this region occur through contact with HIV-infected individuals from other regions. In some areas of Europe, such as the Baltic countries, the most common route of HIV transmission is through injecting drug use and heterosexual sex, including paid sex.

The situation with the spread of HIV/AIDS in Russia is described by some researchers as an epidemic. The first cases of human immunodeficiency virus infection were recorded in the USSR in 1985-1987. Patient zero is officially considered to be a military interpreter who worked in Tanzania in the early 1980s and was infected by a local man during sexual contact. After 1988—1989 Elista HIV outbreak, the disease became known to the general public and the first AIDS centers were established. In 1995-1996, the virus spread among injecting drug users (IDUs) and soon expanded throughout the country. By 2006, HIV had spread beyond the vulnerable IDU group, endangering their heterosexual partners and potentially the entire population.
Kenya has a severe, generalized HIV epidemic, but in recent years, the country has experienced a notable decline in HIV prevalence, attributed in part to significant behavioral change and increased access to ARV. Adult HIV prevalence is estimated to have fallen from 10 percent in the late 1990s to about 4.8 percent in 2017. Women face considerably higher risk of HIV infection than men but have longer life expectancies than men when on ART. The 7th edition of AIDS in Kenya reports an HIV prevalence rate of eight percent in adult women and four percent in adult men. Populations in Kenya that are especially at risk include injecting drug users and people in prostitution, whose prevalence rates are estimated at 53 percent and 27 percent, respectively. Men who have sex with men (MSM) are also at risk at a prevalence of 18.2%. Other groups also include discordant couples however successful ARV-treatment will prevent transmission. Other groups at risk are prison communities, uniformed forces, and truck drivers.
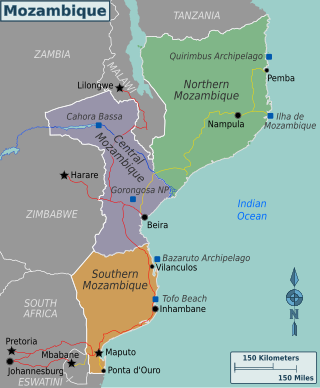
Mozambique is a country particularly hard-hit by the HIV/AIDS epidemic. According to 2008 UNAIDS estimates, this southeast African nation has the 8th highest HIV rate in the world. With 1,600,000 Mozambicans living with HIV, 990,000 of which are women and children, Mozambique's government realizes that much work must be done to eradicate this infectious disease. To reduce HIV/AIDS within the country, Mozambique has partnered with numerous global organizations to provide its citizens with augmented access to antiretroviral therapy and prevention techniques, such as condom use. A surge toward the treatment and prevention of HIV/AIDS in women and children has additionally aided in Mozambique's aim to fulfill its Millennium Development Goals (MDGs). Nevertheless, HIV/AIDS has made a drastic impact on Mozambique; individual risk behaviors are still greatly influenced by social norms, and much still needs to be done to address the epidemic and provide care and treatment to those in need.
HIV/AIDS is considered the deadliest epidemic in the 21st century. It is transmitted through sex, intravenous drug use and mother-to-child transmission. Zambia is experiencing a generalized HIV/AIDS epidemic, with a national HIV prevalence rate of 11.3% among adults ages 15 to 49 as of 2018. Per the 2000 Zambian census, the people affected by HIV/AIDS constituted 15% of the total population, amounting to one million, of which 60% were women. The pandemic results in increased number of orphans, with an estimated 600,000 orphans in the country. It was prevalent more in urban areas compared to rural and among all provinces, Copperbelt Province and Lusaka Province had higher occurrence.
The Philippines has one of the lowest rates of infection of HIV/AIDS, yet has one of the fastest growing number of cases worldwide. The Philippines is one of seven countries with growth in number of cases of over 25%, from 2001 to 2009.
In 2016, the prevalence rate of HIV/AIDS in adults aged 15–49 was 0.3%, relatively low for a developing country. This low prevalence has been maintained, as in 2006, the HIV prevalence in Mexico was estimated at around 0.3% as well. The infected population is remains mainly concentrated among high risk populations, men who have sex with other men, intravenous drug users, and commercial sex workers. This low national prevalence is not reflected in the high-risk populations. The prison population in Mexico, faces a fairly similar low rate of around 0.7%. Among the population of prisoners, around 2% are known to be infected with HIV. Sex workers, male and female, face an HIV prevalence of around 7%. Identifying gay men and men who have sex with other men have a prevalence of 17.4%. The highest risk-factor group is identifying transgender people; about 17.4% of this population is known to be infected with HIV. Around 90% of new infections occur by sex-related methods of transmission. Of these known infected populations, around 60% of living infected people are known to be on anti-retroviral therapy (ART).
With less than 1 percent of the population estimated to be HIV-positive, Egypt is a low-HIV-prevalence country. However, between the years 2006 and 2011, HIV prevalence rates in Egypt increased tenfold. Until 2011, the average number of new cases of HIV in Egypt was 400 per year. But, in 2012 and 2013 it increased to about 600 new cases and in 2014 it reached 880 new cases per year. According to UNAIDS 2016 statistics, there are about 11,000 people currently living with HIV in Egypt. The Ministry of Health and Population reported in 2020 over 13,000 Egyptians are living with HIV/AIDS. However, unsafe behaviors among most-at-risk populations and limited condom usage among the general population place Egypt at risk of a broader epidemic.
Despite big declines, the prevalence of HIV/AIDS in Cambodia is among the highest in Asia. Although Cambodia is one of the poorest countries in the world, extensive HIV prevention and control efforts by the Royal Government of Cambodia and its partners have helped to reduce the spread of HIV. Between 2003 and 2005, the estimated HIV prevalence among Cambodian adults aged 15 to 49 declined by 20%, from 2.0% to 1.6%. As of 2019, 0.6% of Cambodian adults currently has the virus.

With an estimated 150,000 people living with HIV/AIDS in 2016, Haiti has the most overall cases of HIV/AIDS in the Caribbean and its HIV prevalence rates among the highest percentage-wise in the region. There are many risk-factor groups for HIV infection in Haiti, with the most common ones including lower socioeconomic status, lower educational levels, risky behavior, and lower levels of awareness regarding HIV and its transmission.
HIV prevention refers to practices that aim to prevent the spread of the human immunodeficiency virus (HIV). HIV prevention practices may be undertaken by individuals to protect their own health and the health of those in their community, or may be instituted by governments and community-based organizations as public health policies.
Children in Uganda are regularly exposed to many preventable health risks. According to the WHO, the country ranks 186th out of 191 eligible countries in life expectancy. The country also ranks 168 out of 188 in infant mortality rates, with a lower rank reflecting lower infant mortality. There are also about 97 infant mortalities out of 1,000. There are many cultural factors influencing the current health status of Uganda including the negative stigmas associated with sex, and the wood-burning stoves. The former of these has resulted in a severe lack in education and communication necessary to improve the health and well-being of children. There are multiple factors negatively impacting the health of children in Uganda. Those factors include HIV/AIDS, malnutrition, lack of sanitation, vaccinations, insufficient drugs, and an insufficient number of motivated healthcare workers. The World Health Organization attributes the tragic situation to wars that occurred before 1986 as well as the HIV/AIDS epidemic. The HIV/AIDS epidemic has resulted mainly from the mother-to-child transmission that spreads from one generation to the next, which could have easily been prevented from educating mothers and providing them with medical treatment. Medical treatment could protect them and their children. The knowledge of HIV, how people can contract it, their individual HIV status and counseling for the disease. These are several factors that assist in the prevention of HIV/AIDS and the HIV/AIDS epidemic, which is the leading cause of the detrimental state of child health in Uganda.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.
Treatment as prevention (TasP) is a concept in public health that promotes treatment as a way to prevent and reduce the likelihood of HIV illness, death and transmission from an infected individual to others. Expanding access to earlier HIV diagnosis and treatment as a means to address the global epidemic by preventing illness, death and transmission was first proposed in 2000 by Garnett et al. The term is often used to talk about treating people that are currently living with human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) to prevent illness, death and transmission. Although some experts narrow this to only include preventing infections, treatment prevents illnesses such as tuberculosis and has been shown to prevent death. The dual impact on well-being and its 100% effectiveness in reducing transmission makes TasP the most important element in the HIV prevention toolkit. In relation to HIV, antiretroviral therapy (ART) is a three or more drug combination therapy that is used to decrease the viral load, or the measured amount of virus, in an infected individual. Such medications are used as a preventative for infected individuals to not only spread the HIV virus to their negative partners but also improve their current health to increase their lifespans. Other names for ART include highly active antiretroviral therapy (HAART), combination antiretroviral therapy (cART), triple therapy and triple drug cocktail. When taken correctly, ART is able to diminish the presence of the HIV virus in the bodily fluids of an infected person to a level of undetectability. Undetectability ensures that infection does not necessarily have an effect on a person's general health, and that there is no longer a risk of passing along HIV to others. Consistent adherence to an ARV regimen, monitoring, and testing are essential for continued confirmed viral suppression. Treatment as prevention rose to great prominence in 2011, as part of the HPTN 052 study, which shed light on the benefits of early treatment for HIV positive individuals.
References
- 1 2 "WHO declares HIV outbreak in Larkana as 'Grade 2 Emergency'". The News International. 8 June 2019.
- 1 2 3 ur-Rehman, Zia; Abi-Habib, Maria (26 October 2019). "Panic in Pakistani City After 900 Children Test Positive for H.I.V." New York Times.
- ↑ "Reused Syringes, Drips Infected Hundreds of Pakistani Children With HIV". Wall Street Journal. 14 June 2019. Retrieved 26 October 2019.
- ↑ "PAKISTAN'S 'POSITIVE' CRISIS". Dawn. Dec 7, 2019.
- 1 2 Arif, Fizzah (July 2019). "HIV crisis in Sindh, Pakistan: the tip of the iceberg". Lancet Infectious Diseases. 19 (7): 695–696. doi: 10.1016/S1473-3099(19)30265-8 . PMID 31250819. S2CID 195760327 . Retrieved 16 January 2021.
- ↑ "Responding to the HIV outbreak in Larkana". unaids.org. Retrieved 16 January 2021.