Neurosurgery or neurological surgery, known in common parlance as brain surgery, is the medical specialty concerned with the surgical treatment of disorders which affect any portion of the nervous system including the brain, spinal cord and peripheral nervous system.
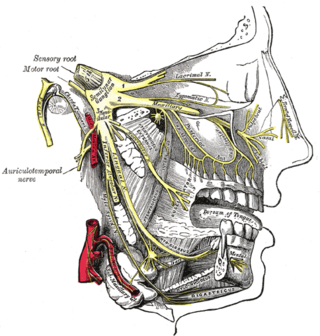
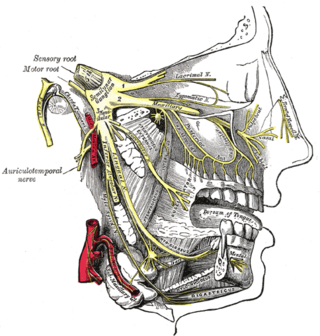
Trigeminal neuralgia, also called Fothergill disease, tic douloureux, trifacial neuralgia, or suicide disease, is a long-term pain disorder that affects the trigeminal nerve, the nerve responsible for sensation in the face and motor functions such as biting and chewing. It is a form of neuropathic pain. There are two main types: typical and atypical trigeminal neuralgia. The typical form results in episodes of severe, sudden, shock-like pain in one side of the face that lasts for seconds to a few minutes. Groups of these episodes can occur over a few hours. The atypical form results in a constant burning pain that is less severe. Episodes may be triggered by any touch to the face. Both forms may occur in the same person. It is regarded as one of the most painful disorders known to medicine, and often results in depression and suicide.
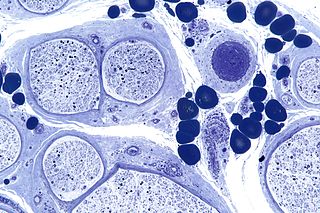
Diabetic neuropathy is various types of nerve damage associated with diabetes mellitus. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from a microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.
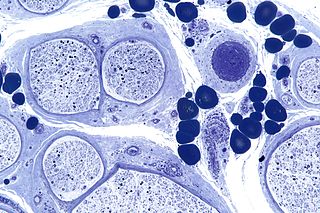
Peripheral neuropathy, often shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerve fibers are affected. Neuropathies affecting motor, sensory, or autonomic nerve fibers result in different symptoms. More than one type of fiber may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

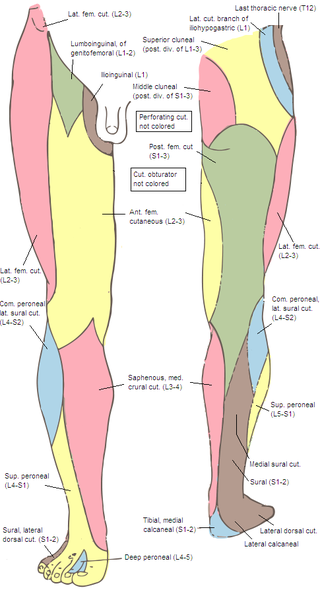
Peroneal nerve paralysis is a paralysis on common fibular nerve that affects patient’s ability to lift the foot at the ankle. The condition was named after Friedrich Albert von Zenker. Peroneal nerve paralysis usually leads to neuromuscular disorder, peroneal nerve injury, or foot drop which can be symptoms of more serious disorders such as nerve compression. The origin of peroneal nerve palsy has been reported to be associated with musculoskeletal injury or isolated nerve traction and compression. Also it has been reported to be mass lesions and metabolic syndromes. Peroneal nerve is most commonly interrupted at the knee and possibly at the joint of hip and ankle. Most studies reported that about 30% of peroneal nerve palsy is followed from knee dislocations.

Tarsal tunnel syndrome (TTS) is a nerve entrapment syndrome causing a painful foot condition in which the tibial nerve is compressed as it travels through the tarsal tunnel. This tunnel is found along the inner leg behind the medial malleolus. The posterior tibial artery, tibial nerve, and tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles travel in a bundle through the tarsal tunnel. Inside the tunnel, the nerve splits into three segments. One nerve (calcaneal) continues to the heel, the other two continue on to the bottom of the foot. The tarsal tunnel is delineated by bone on the inside and the flexor retinaculum on the outside.
The common fibular nerve is a nerve in the lower leg that provides sensation over the posterolateral part of the leg and the knee joint. It divides at the knee into two terminal branches: the superficial fibular nerve and deep fibular nerve, which innervate the muscles of the lateral and anterior compartments of the leg respectively. When the common fibular nerve is damaged or compressed, foot drop can ensue.
Hand surgery deals with both surgical and non-surgical treatment of conditions and problems that may take place in the hand or upper extremity including injury and infection. Hand surgery may be practiced by post graduates of orthopedic surgery and plastic surgery.

The sural nerve(L4-S1) is generally considered a pure cutaneous nerve of the posterolateral leg to the lateral ankle. The sural nerve originates from a combination of either the sural communicating branch and medial sural cutaneous nerve, or the lateral sural cutaneous nerve. This group of nerves is termed the sural nerve complex. There are eight documented variations of the sural nerve complex. Once formed the sural nerve takes its course midline posterior to posterolateral around the lateral malleolus. The sural nerve terminates as the lateral dorsal cutaneous nerve.
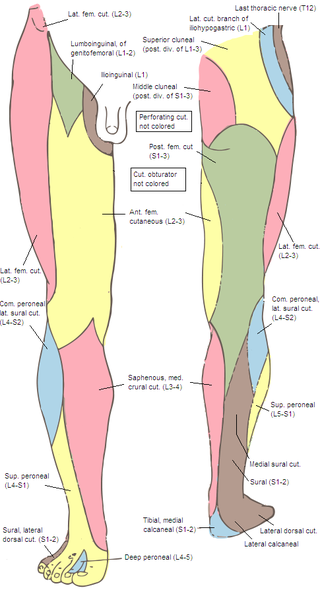
The superior cluneal nerves are pure sensory nerves that innervate the skin of the upper part of the buttocks. They are the terminal ends of the L1-L3 spinal nerve dorsal rami lateral branches. They are one of three different types of cluneal nerves. They travel inferiorly through multiple layers of muscles, then traverse osteofibrous tunnels between the thoracolumbar fascia and iliac crest.

Idiopathic Ulnar neuropathy at the elbow is a condition where pressure on the ulnar nerve as it passes through the cubital tunnel causes nerve dysfunction (neuropathy). The symptoms of neuropathy are paresthesia (tingling) and numbness primarily affecting the little finger and ring finger of the hand. Ulnar neuropathy can progress to weakness and atrophy of the muscles in the hand. Symptoms can be alleviated by attempts to keep the elbow from flexing while sleeping, such as sticking one's arm in the pillow case, so the pillow restricts flexion.

Radial tunnel syndrome (RTS) is a compression neuropathy of the radial nerve as it travels from the upper arm to the hand and wrist.
Anterior interosseous syndrome is a medical condition in which damage to the anterior interosseous nerve (AIN), a distal motor and sensory branch of the median nerve, classically with severe weakness of the pincer movement of the thumb and index finger, and can cause transient pain in the wrist.

Pronator teres syndrome is a compression neuropathy of the median nerve at the elbow. It is rare compared to compression at the wrist or isolated injury of the anterior interosseous branch of the median nerve.

Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. The diagnosis is largely clinical and can be confirmed with diagnostic nerve blocks. Occasionally imaging and electrophysiology studies aid in the diagnosis. Timely diagnosis is important as untreated chronic nerve compression may cause permanent damage. A surgical nerve decompression can relieve pressure on the nerve but cannot always reverse the physiological changes that occurred before treatment. Nerve injury by a single episode of physical trauma is in one sense an acute compression neuropathy but is not usually included under this heading, as chronic compression takes a unique pathophysiological course.

Carpal tunnel surgery, also called carpal tunnel release (CTR) and carpal tunnel decompression surgery, is a nerve decompression in which the transverse carpal ligament is divided. It is a surgical treatment for carpal tunnel syndrome (CTS) and recommended when there is constant (not just intermittent) numbness, muscle weakness, or atrophy, and when night-splinting no longer controls intermittent symptoms of pain in the carpal tunnel. In general, milder cases can be controlled for months to years, but severe cases are unrelenting symptomatically and are likely to result in surgical treatment. Approximately 500,000 surgical procedures are performed each year, and the economic impact of this condition is estimated to exceed $2 billion annually.
Ischemic monomelic neuropathy(IMN) is an uncommon vascular access complication in hemodialysis patients that manifests as multiple mononeuropathies without clinical ischemia. Ischemic monomelic neuropathy is most likely to affect patients who have had brachiocephalic vascular grafts, and it is characterized by symptoms of acute pain, numbness, and paresthesia in addition to motor weakness. The term "ischemic monomelic neuropathy" was first used in 1983 by Wilbourn, despite the fact that Bolton et al. had originally reported on it in 1979.
Michael James Polydefkis is an American neurologist. He is a Professor of Neurology at Johns Hopkins University School of Medicine and Co-Director of the Cutaneous Nerve Laboratory. Polydefkis research focuses on treating hATTR amyloidosis and diabetic and HIV-associated peripheral neuropathy.

Susan E. Mackinnon is a Canadian plastic and reconstructive surgeon who is a pioneer in the field of peripheral nerve transfer and regeneration. She performed the world's first nerve allotransplantation in 1988. She is a past president of the American Association of Plastic Surgeons, the Plastic Surgery Research Council, and the American Association of Hand Surgery. As of 2022, she is the Minot Packer Fryer Professor of Plastic Surgery at Washington University School of Medicine in St. Louis, United States.
A nerve decompression is a neurosurgical procedure to relieve chronic, direct pressure on a nerve to treat nerve entrapment, a pain syndrome characterized by severe chronic pain and muscle weakness. In this way a nerve decompression targets the underlying pathophysiology of the syndrome and is considered a first-line surgical treatment option for peripheral nerve pain. Despite treating the underlying cause of the disease, the symptoms may not be fully reversible as delays in diagnosis can allow permanent damage to occur to the nerve and surrounding microvasculature. Traditionally only nerves accessible with open surgery have been good candidates, however innovations in laparoscopy and nerve-sparing techniques made nearly all nerves in the body good candidates, as surgical access is no longer a barrier.