Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction.

Laryngoscopy is endoscopy of the larynx, a part of the throat. It is a medical procedure that is used to obtain a view, for example, of the vocal folds and the glottis. Laryngoscopy may be performed to facilitate tracheal intubation during general anaesthesia or cardiopulmonary resuscitation or for surgical procedures on the larynx or other parts of the upper tracheobronchial tree.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
A tracheal tube is a catheter that is inserted into the trachea for the primary purpose of establishing and maintaining a patent airway and to ensure the adequate exchange of oxygen and carbon dioxide.
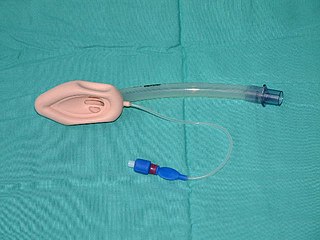
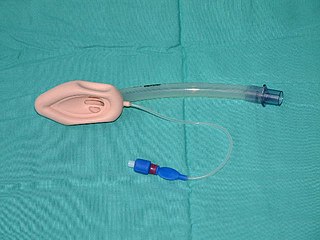
A laryngeal mask airway (LMA), also known as laryngeal mask, is a medical device that keeps a patient's airway open during anaesthesia or while they are unconscious. It is a type of supraglottic airway device. They are most commonly used by anaesthetists to channel oxygen or inhalational anaesthetic to the lungs during surgery and in the pre-hospital setting for unconscious patients.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).

Respiratory arrest is a medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.
In anaesthesia and advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.

In anesthesia, the Mallampati score or Mallampati classification, named after the Indian anaesthesiologist Seshagiri Mallampati, is used to predict the ease of endotracheal intubation. The test comprises a visual assessment of the distance from the tongue base to the roof of the mouth, and therefore the amount of space in which there is to work. It is an indirect way of assessing how difficult an intubation will be; this is more definitively scored using the Cormack-Lehane classification system, which describes what is actually seen using direct laryngoscopy during the intubation process itself. A high Mallampati score is associated with more difficult intubation as well as a higher incidence of sleep apnea.

Sir Robert Reynolds Macintosh was a New Zealand-born British anaesthetist. He was the first professor of anaesthetics outside the United States.
Cricoid pressure, also known as the Sellick manoeuvre or Sellick maneuver, is a technique used in endotracheal intubation to try to reduce the risk of regurgitation. The technique involves the application of pressure to the cricoid cartilage at the neck, thus occluding the esophagus which passes directly behind it.

Throughout recorded history, attempts at producing a state of general anesthesia can be traced back to the writings of ancient Sumerians, Babylonians, Assyrians, Egyptians, Indians, and Chinese. Despite significant advances in anatomy and surgical technique during the Renaissance, surgery remained a last-resort treatment largely due to the pain associated with it. However, scientific discoveries in the late 18th and early 19th centuries paved the way for the development of modern anesthetic techniques.
Tracheal intubation, an invasive medical procedure, is the placement of a flexible plastic catheter into the trachea. For millennia, tracheotomy was considered the most reliable method of tracheal intubation. By the late 19th century, advances in the sciences of anatomy and physiology, as well as the beginnings of an appreciation of the germ theory of disease, had reduced the morbidity and mortality of this operation to a more acceptable rate. Also in the late 19th century, advances in endoscopic instrumentation had improved to such a degree that direct laryngoscopy had finally become a viable means to secure the airway by the non-surgical orotracheal route. Nasotracheal intubation was not widely practiced until the early 20th century. The 20th century saw the transformation of the practices of tracheotomy, endoscopy and non-surgical tracheal intubation from rarely employed procedures to essential components of the practices of anesthesia, critical care medicine, emergency medicine, gastroenterology, pulmonology and surgery.
The Cormack-Lehane system classifies views obtained by direct laryngoscopy based on the structures seen. It was initially described by R.S. Cormack and J. Lehane in 1984 as a way of simulating potential scenarios that trainee anaesthetists might face. A modified version that subdivided Grade 2 was initially described in 1998.

The laryngeal tube is an airway management device designed as an alternative to other airway management techniques such as mask ventilation, laryngeal mask airway, and tracheal intubation. This device can be inserted blindly through the oropharynx into the hypopharynx to create an airway during anaesthesia and cardiopulmonary resuscitation so as to enable mechanical ventilation of the lungs.

A double-lumen endotracheal tube is a type of endotracheal tube which is used in tracheal intubation during thoracic surgery and other medical conditions to achieve selective, one-sided ventilation of either the right or the left lung.
An bronchial blocker is a device which can be inserted down a tracheal tube after tracheal intubation so as to block off the right or left main bronchus of the lungs in order to be able to achieve a controlled one sided ventilation of the lungs in thoracic surgery. The lung tissue distal to the obstruction will collapse, thus allowing the surgeon's view and access to relevant structures within the thoracic cavity.

Advanced airway management is the subset of airway management that involves advanced training, skill, and invasiveness. It encompasses various techniques performed to create an open or patent airway – a clear path between a patient's lungs and the outside world.

Intubation granuloma is a benign growth of granulation tissue in the larynx or trachea, which arises from tissue trauma due to endotracheal intubation. This medical condition is described as a common late complication of tracheal intubation, specifically caused by irritation to the mucosal tissue of the airway during insertion or removal of the patient's intubation tube.

Suction Assisted Laryngoscopy Airway Decontamination (SALAD) is incremental step-wise approach to the management of a massively contaminated airway.