Glycogen storage disease type V, also known as McArdle's disease, is a metabolic disorder, more specifically a muscle glycogen storage disease, caused by a deficiency of myophosphorylase. Its incidence is reported as one in 100,000, roughly the same as glycogen storage disease type I.

Rhabdomyolysis is a condition in which damaged skeletal muscle breaks down rapidly. Symptoms may include muscle pains, weakness, vomiting, and confusion. There may be tea-colored urine or an irregular heartbeat. Some of the muscle breakdown products, such as the protein myoglobin, are harmful to the kidneys and may lead to kidney failure.

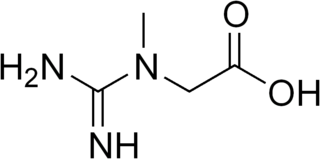
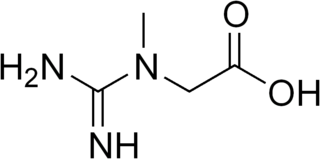
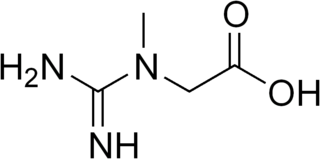
Creatine ( or ) is an organic compound with the nominal formula (H2N)(HN)CN(CH3)CH2CO2H. This species exists in various modifications (tautomers) in solution. Creatine is found in vertebrates where it facilitates recycling of adenosine triphosphate (ATP), primarily in muscle and brain tissue. Recycling is achieved by converting adenosine diphosphate (ADP) back to ATP via donation of phosphate groups. Creatine also acts as a buffer.
Encephalopathy means any disorder or disease of the brain, especially chronic degenerative conditions. In modern usage, encephalopathy does not refer to a single disease, but rather to a syndrome of overall brain dysfunction; this syndrome has many possible organic and inorganic causes.

Phosphocreatine, also known as creatine phosphate (CP) or PCr (Pcr), is a phosphorylated creatine molecule that serves as a rapidly mobilizable reserve of high-energy phosphates in skeletal muscle, myocardium and the brain to recycle adenosine triphosphate, the energy currency of the cell.

Hypotonia is a state of low muscle tone, often involving reduced muscle strength. Hypotonia is not a specific medical disorder, but a potential manifestation of many different diseases and disorders that affect motor nerve control by the brain or muscle strength. Hypotonia is a lack of resistance to passive movement, whereas muscle weakness results in impaired active movement. Central hypotonia originates from the central nervous system, while peripheral hypotonia is related to problems within the spinal cord, peripheral nerves and/or skeletal muscles. Severe hypotonia in infancy is commonly known as floppy baby syndrome. Recognizing hypotonia, even in early infancy, is usually relatively straightforward, but diagnosing the underlying cause can be difficult and often unsuccessful. The long-term effects of hypotonia on a child's development and later life depend primarily on the severity of the muscle weakness and the nature of the cause. Some disorders have a specific treatment but the principal treatment for most hypotonia of idiopathic or neurologic cause is physical therapy and/or occupational therapy for remediation.
Lesch–Nyhan syndrome (LNS) is a rare inherited disorder caused by a deficiency of the enzyme hypoxanthine-guanine phosphoribosyltransferase (HGPRT). This deficiency occurs due to mutations in the HPRT1 gene located on the X chromosome. LNS affects about 1 in 380,000 live births. The disorder was first recognized and clinically characterized by American medical student Michael Lesch and his mentor, pediatrician William Nyhan, at Johns Hopkins.

Mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes (MELAS) is one of the family of mitochondrial diseases, which also include MERRF syndrome, and Leber's hereditary optic neuropathy. It was first characterized under this name in 1984. A feature of these diseases is that they are caused by defects in the mitochondrial genome which is inherited purely from the female parent.

Glycine encephalopathy is a rare autosomal recessive disorder of glycine metabolism. After phenylketonuria, glycine encephalopathy is the second most common disorder of amino acid metabolism. The disease is caused by defects in the glycine cleavage system, an enzyme responsible for glycine catabolism. There are several forms of the disease, with varying severity of symptoms and time of onset. The symptoms are exclusively neurological in nature, and clinically this disorder is characterized by abnormally high levels of the amino acid glycine in bodily fluids and tissues, especially the cerebrospinal fluid.

L-Arginine:glycine amidinotransferase is the enzyme that catalyses the transfer of an amidino group from L-arginine to glycine. The products are L-ornithine and glycocyamine, also known as guanidinoacetate, the immediate precursor of creatine. Creatine and its phosphorylated form play a central role in the energy metabolism of muscle and nerve tissues. Creatine is in highest concentrations in the skeletal muscle, heart, spermatozoa and photoreceptor cells. Creatine helps buffer the rapid changes in ADP/ATP ratio in muscle and nerve cells during active periods. Creatine is also synthesized in other tissues, such as pancreas, kidneys, and liver, where amidinotransferase is located in the cytoplasm, including the intermembrane space of the mitochondria, of the cells that make up those tissues.
Guanidinoacetate methyltransferase deficiency, is an autosomal recessive cerebral creatine deficiency that primarily affects the nervous system and muscles. It is the first described disorder of creatine metabolism, and results from deficient activity of guanidinoacetate methyltransferase, an enzyme involved in the synthesis of creatine. Clinically, affected individuals often present with hypotonia, seizures and developmental delay. Diagnosis can be suspected on clinical findings, and confirmed by specific biochemical tests, brain magnetic resonance spectroscopy, or genetic testing. Biallelic pathogenic variants in GAMT are the underlying cause of the disorder. After GAMT deficiency is diagnosed, it can be treated by dietary adjustments, including supplementation with creatine. Treatment is highly effective if started early in life. If treatment is started late, it cannot reverse brain damage which has already taken place.
Cerebral creatine deficiencies are a small group of inherited disorders that result from defects in creatine biosynthesis and utilization. Commonly affected tissues include the brain and muscles. There are three distinct CCDs. The most common is creatine transporter defect (CTD), an X-linked disorder caused by pathogenic variants in SLC6A8. The main symptoms of CTD are intellectual disability and developmental delay, and these are caused by a lack of creatine in the brain, due to the defective transporter. There are also two enzymatic defects of creatine biosynthesis, arginine:glycine amidinotransferase deficiency, caused by variants in GATM and guanidinoacetate methyltransferase deficiency, caused by variants in GAMT. The single enzyme defects are both inherited in an autosomal recessive manner.

Glycine amidinotransferase, mitochondrial is an enzyme that in humans is encoded by the GATM gene.

Glycocyamine is a metabolite of glycine in which the amino group has been converted into a guanidine by guanylation. In vertebrate organism it is then transformed into creatine by methylation.

Jansky–Bielschowsky disease is an extremely rare autosomal recessive genetic disorder that is part of the neuronal ceroid lipofuscinosis (NCL) family of neurodegenerative disorders. It is caused by the accumulation of lipopigments in the body due to a deficiency in tripeptidyl peptidase I as a result of a mutation in the TPP1 gene. Symptoms appear between ages 2 and 4 and consist of typical neurodegenerative complications: loss of muscle function (ataxia), drug resistant seizures (epilepsy), apraxia, development of muscle twitches (myoclonus), and vision impairment. This late-infantile form of the disease progresses rapidly once symptoms are onset and ends in death between age 8 and teens. The prevalence of Jansky–Bielschowsky disease is unknown, however NCL collectively affects an estimated 1 in 100,000 individuals worldwide. Jansky–Bielschowsky disease is related to late-infantile Batten disease and LINCL, and is under the umbrella of neuronal ceroid lipofuscinosis.

Ornithine aminotransferase deficiency is an inborn error of ornithine metabolism, caused by decreased activity of the enzyme ornithine aminotransferase. Biochemically, it can be detected by elevated levels of ornithine in the blood. Clinically, it presents initially with poor night vision, which slowly progresses to total blindness. It is believed to be inherited in an autosomal recessive manner. Approximately 200 known cases have been reported in the literature. The incidence is highest in Finland, estimated at 1:50,000.
Sepiapterin reductase deficiency is an inherited pediatric disorder characterized by movement problems, and most commonly displayed as a pattern of involuntary sustained muscle contractions known as dystonia. Symptoms are usually present within the first year of age, but diagnosis is delayed due to physicians lack of awareness and the specialized diagnostic procedures. Individuals with this disorder also have delayed motor skills development including sitting, crawling, and need assistance when walking. Additional symptoms of this disorder include intellectual disability, excessive sleeping, mood swings, and an abnormally small head size. SR deficiency is a very rare condition. The first case was diagnosed in 2001, and since then there have been approximately 30 reported cases. At this time, the condition seems to be treatable, but due to a lack of overall awareness and a series of atypical procedures used to diagnose this condition pose a dilemma.
Creatine Transporter Deficiency (CTD) is an inborn error of creatine metabolism in which creatine is not properly transported to the brain and muscles due to defective creatine transporters. CTD is an X-linked disorder caused by mutation in SLC6A8. SLC6A8 is located at Xq28. Hemizygous males with CTD express speech and behavior abnormalities, intellectual disabilities, development delay, seizures, and autistic behavior. Heterozygous females with CTD generally express fewer, less severe symptoms. CTD is one of three different types of cerebral creatine deficiency (CCD). The other two types of CCD are guanidinoacetate methyltransferase (GAMT) deficiency and L-arginine:glycine amidinotransferase (AGAT) deficiency. Clinical presentation of CTD is similar to that of GAMT and AGAT deficiency. CTD was first identified in 2001 with the presence of a hemizygous nonsense change in SLC6A8 in a male patient.

NGLY1 deficiency is a very rare genetic disorder caused by biallelic pathogenic variants in NGLY1. It is an autosomal recessive disorder. Errors in deglycosylation are responsible for the symptoms of this condition. Clinically, most affected individuals display developmental delay, lack of tears, elevated liver transaminases and a movement disorder. NGLY1 deficiency is difficult to diagnose, and most individuals have been identified by exome sequencing.

Acyl-CoA oxidase deficiency is a rare disorder that leads to significant damage and deterioration of nervous system functions (neurodegeneration). It is caused by pathogenic variants in ACOX1, which codes for the production of an enzyme called peroxisomal straight-chain acyl-CoA oxidase (ACOX1). This specific enzyme is responsible for the breakdown of very long chain fatty acids (VLCFAs).