The sacrum, in human anatomy, is a large, triangular bone at the base of the spine that forms by the fusing of the sacral vertebrae (S1–S5) between ages 18 and 30.

The lumbar vertebrae are located between the thoracic vertebrae and pelvis. They form the lower part of the human back in humans, and the tail end of the back in quadrupeds. In humans, there are five lumbar vertebrae. The term is used to describe the anatomy of humans and quadrupeds, such as horses, pigs, or cattle. These bones are found in particular cuts of meat, including tenderloin or sirloin steak.

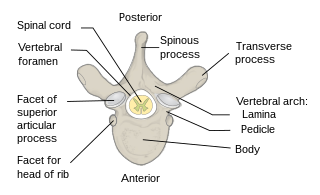
A laminectomy is a surgical procedure that removes a portion of a vertebra called the lamina, which is the roof of the spinal canal. It is a major spine operation with residual scar tissue and may result in postlaminectomy syndrome. Depending on the problem, more conservative treatments may be viable.

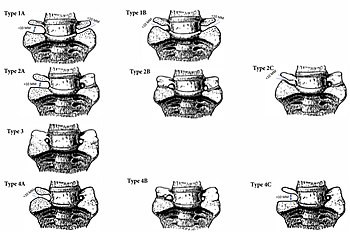
Spondylolisthesis is the displacement of one spinal vertebra compared to another. While some medical dictionaries define spondylolisthesis specifically as the forward or anterior displacement of a vertebra over the vertebra inferior to it, it is often defined in medical textbooks as displacement in any direction. Spondylolisthesis is graded based upon the degree of slippage of one vertebral body relative to the subsequent adjacent vertebral body. Spondylolisthesis is classified as one of the six major etiologies: degenerative, traumatic, dysplastic, isthmic, pathologic, or post-surgical. Spondylolisthesis most commonly occurs in the lumbar spine, primarily at the L5-S1 level, with the L5 vertebral body anteriorly translating over the S1 vertebral body.

Cauda equina syndrome (CES) is a condition that occurs when the bundle of nerves below the end of the spinal cord known as the cauda equina is damaged. Signs and symptoms include low back pain, pain that radiates down the leg, numbness around the anus, and loss of bowel or bladder control. Onset may be rapid or gradual.

Klippel–Feil syndrome (KFS), also known as cervical vertebral fusion syndrome, is a rare congenital condition characterized by the abnormal fusion of any two of the seven bones in the neck. It can result in a limited ability to move the neck and shortness of the neck, resulting in the appearance of a low hairline. Most people only have one or two of those symptoms so it may not be noticeable without medical imaging.

The multifidusmuscle consists of a number of fleshy and tendinous fasciculi, which fill up the groove on either side of the spinous processes of the vertebrae, from the sacrum to the axis. While very thin, the multifidus muscle plays an important role in stabilizing the joints within the spine. The multifidus is one of the transversospinales.

Spinal fusion, also called spondylodesis or spondylosyndesis, is a surgery performed by orthopaedic surgeons or neurosurgeons that joins two or more vertebrae. This procedure can be performed at any level in the spine and prevents any movement between the fused vertebrae. There are many types of spinal fusion and each technique involves using bone grafting—either from the patient (autograft), donor (allograft), or artificial bone substitutes—to help the bones heal together. Additional hardware is often used to hold the bones in place while the graft fuses the two vertebrae together. The placement of hardware can be guided by fluoroscopy, navigation systems, or robotics.

The conus medullaris or conus terminalis is the tapered, lower end of the spinal cord. It occurs near lumbar vertebral levels 1 (L1) and 2 (L2), occasionally lower. The upper end of the conus medullaris is usually not well defined, however, its corresponding spinal cord segments are usually S1–S5.
Congenital vertebral anomalies are a collection of malformations of the spine. Most, around 85%, are not clinically significant, but they can cause compression of the spinal cord by deforming the vertebral canal or causing instability. This condition occurs in the womb. Congenital vertebral anomalies include alterations of the shape and number of vertebrae.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.

Diastematomyelia is a congenital disorder in which a part of the spinal cord is split, usually at the level of the upper lumbar vertebra in the longitudinal (sagittal) direction. Females are affected much more commonly than males. This condition occurs in the presence of an osseous, cartilaginous or fibrous septum in the central portion of the spinal canal which then produces a complete or incomplete sagittal division of the spinal cord into two hemicords. When the split does not reunite distally to the spur, the condition is referred to as diplomyelia, which is true duplication of the spinal cord.

A laminotomy is an orthopaedic neurosurgical procedure that removes part of the lamina of a vertebral arch in order to relieve pressure in the vertebral canal. A laminotomy is less invasive than conventional vertebral column surgery techniques, such as laminectomy because it leaves more ligaments and muscles attached to the spinous process intact and it requires removing less bone from the vertebra. As a result, laminotomies typically have a faster recovery time and result in fewer postoperative complications. Nevertheless, possible risks can occur during or after the procedure like infection, hematomas, and dural tears. Laminotomies are commonly performed as treatment for lumbar spinal stenosis and herniated disks. MRI and CT scans are often used pre- and post surgery to determine if the procedure was successful.

The spinal cord is a long, thin, tubular structure made up of nervous tissue that extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column (backbone) of vertebrate animals. The center of the spinal cord is hollow and contains a structure called the central canal, which contains cerebrospinal fluid. The spinal cord is also covered by meninges and enclosed by the neural arches. Together, the brain and spinal cord make up the central nervous system.

Facet syndrome is a syndrome in which the facet joints cause painful symptoms. In conjunction with degenerative disc disease, a distinct but functionally related condition, facet arthropathy is believed to be one of the most common causes of lower back pain.

Tarlov cysts, are type II innervated meningeal cysts, cerebrospinal-fluid-filled (CSF) sacs most frequently located in the spinal canal of the sacral region of the spinal cord (S1–S5) and much less often in the cervical, thoracic or lumbar spine. They can be distinguished from other meningeal cysts by their nerve-fiber-filled walls. Tarlov cysts are defined as cysts formed within the nerve-root sheath at the dorsal root ganglion. The etiology of these cysts is not well understood; some current theories explaining this phenomenon have not yet been tested or challenged but include increased pressure in CSF, filling of congenital cysts with one-way valves, inflammation in response to trauma and disease. They are named for American neurosurgeon Isadore Tarlov, who described them in 1938.

The vertebral column, also known as the spinal column, spine or backbone, is the core part of the axial skeleton in vertebrate animals. The vertebral column is the defining and eponymous characteristic of the vertebrate endoskeleton, where the notochord found in all chordates has been replaced by a segmented series of mineralized irregular bones called vertebrae, separated by fibrocartilaginous intervertebral discs. The dorsal portion of the vertebral column houses the spinal canal, an elongated cavity formed by alignment of the vertebral neural arches that encloses and protects the spinal cord, with spinal nerves exiting via the intervertebral foramina to innervate each body segments.
Each vertebra is an irregular bone with a complex structure composed of bone and some hyaline cartilage, that make up the vertebral column or spine, of vertebrates. The proportions of the vertebrae differ according to their spinal segment and the particular species.
The furcal nerve links the lumbar plexus and the sacral plexus. It has its own dorsal and ventral branches with fibres that branch out to become part of the femoral and obturator nerves. The furcal nerve is found in the lumbosacral trunk most commonly at the level of the fourth lumbar vertebra (L4).
Degenerative lumbosacral stenosis (DLSS), also known as cauda equina syndrome, is a pathologic degeneration in the lumbosacral disk in dogs; affecting the articulation, nerve progression, tissue and joint connections of the disk. This degeneration causes compressions in soft tissues and nerve root locations in the ultimate caudal area of the medulla, causing neuropathic pain in the lumbar vertebrae.