Infant formula, baby formula, or simply formula ; or baby milk or infant milk, is a manufactured food designed and marketed for feeding to babies and infants under 12 months of age, usually prepared for bottle-feeding or cup-feeding from powder or liquid. The U.S. Federal Food, Drug, and Cosmetic Act (FFDCA) defines infant formula as "a food which purports to be or is represented for special dietary use solely as a food for infants by reason of its simulation of human milk or its suitability as a complete or partial substitute for human milk".

A breast pump is a mechanical device that lactating women use to extract milk from their breasts. They may be manual devices powered by hand or foot movements or automatic devices powered by electricity.

Mastitis is inflammation of the breast or udder, usually associated with breastfeeding. Symptoms typically include local pain and redness. There is often an associated fever and general soreness. Onset is typically fairly rapid and usually occurs within the first few months of delivery. Complications can include abscess formation.

Preterm birth, also known as premature birth, is the birth of a baby at fewer than 37 weeks gestational age, as opposed to full-term delivery at approximately 40 weeks. Extreme preterm is less than 28 weeks, very early preterm birth is between 28 and 32 weeks, early preterm birth occurs between 32 and 36 weeks, late preterm birth is between 34 and 36 weeks' gestation. These babies are also known as premature babies or colloquially preemies or premmies. Symptoms of preterm labor include uterine contractions which occur more often than every ten minutes and/or the leaking of fluid from the vagina before 37 weeks. Premature infants are at greater risk for cerebral palsy, delays in development, hearing problems and problems with their vision. The earlier a baby is born, the greater these risks will be.

Breast milk or mother's milk is milk produced by mammary glands located in the breast of a human female. Breast milk is the primary source of nutrition for newborns, containing fat, protein, carbohydrates and variable minerals and vitamins. Breast milk also contains substances that help protect an infant against infection and inflammation, whilst also contributing to healthy development of the immune system and gut microbiome.
Necrotizing enterocolitis (NEC) is a devastating intestinal disease that affects premature or very low birth weight infants. Symptoms may include poor feeding, bloating, decreased activity, blood in the stool, vomiting of bile, bowel death, multiorgan failure, and even death.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.

Chorioamnionitis, also known as intra-amniotic infection (IAI), is inflammation of the fetal membranes, usually due to bacterial infection. In 2015, a National Institute of Child Health and Human Development Workshop expert panel recommended use of the term "triple I" to address the heterogeneity of this disorder. The term triple I refers to intrauterine infection or inflammation or both and is defined by strict diagnostic criteria, but this terminology has not been commonly adopted although the criteria are used.
Gray baby syndrome is a rare but serious, even fatal, side effect that occurs in newborn infants following the accumulation of antibiotic chloramphenicol. Chloramphenicol is a broad-spectrum antibiotic that has been used to treat a variety of bacteria infections like Streptococcus pneumoniae as well as typhoid fever, meningococcal sepsis, cholera, and eye infections. Chloramphenicol works by binding to ribosomal subunits which blocks transfer ribonucleic acid and prevents the synthesis of bacterial proteins. Chloramphenicol has also been used to treat neonates born before 37 weeks of the gestational period for prophylaxis purposes. In 1958, newborns born prematurely due to rupture of the amniotic sac were given chloramphenicol to prevent possible infections, and it was noticed that these newborns had a higher mortality rate compared with those who were not treated with the antibiotic. Over the years, chloramphenicol has been used less in clinical practices due to the risks of toxicity not only to neonates, but also to adults due to the risk of aplastic anemia. Chloramphenicol is now reserved to treat certain severe bacteria infections that were not successfully treated with other antibiotic medications. Signs and symptoms are summarized in the WHO Model Formulary for Children 2010 under the rare adverse effect section of chloramphenicol.
Clostridial necrotizing enteritis (CNE) is a severe and potentially fatal type of food poisoning caused by a β-toxin of Clostridium perfringens, Type C. It occurs in some developing regions, particularly in New Guinea, where it is known as pig-bel. The disease was also documented in Germany following World War II, where it was called Darmbrand (literally "bowel fire," or bowel necrosis). The toxin is normally inactivated by certain proteolytic enzymes and by normal cooking, but when these protections are impeded by diverse factors, and high protein is consumed, the disease can emerge.

Breastfeeding difficulties refers to problems that arise from breastfeeding, the feeding of an infant or young child with milk from a woman's breasts. Although babies have a sucking reflex that enables them to suck and swallow milk, and human breast milk is usually the best source of nourishment for human infants, there are circumstances under which breastfeeding can be problematic, or even in rare instances, contraindicated.

Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be pumped and fed to the infant. The World Health Organization (WHO) recommends that breastfeeding begin within the first hour of a baby's life and continue as often and as much as the baby wants. Health organizations, including the WHO, recommend breastfeeding exclusively for six months. This means that no other foods or drinks, other than vitamin D, are typically given. WHO recommends exclusive breastfeeding for the first 6 months of life, followed by continued breastfeeding with appropriate complementary foods for up to 2 years and beyond. Of the 135 million babies born every year, only 42% are breastfed within the first hour of life, only 38% of mothers practice exclusive breastfeeding during the first six months, and 58% of mothers continue breastfeeding up to the age of two years and beyond.
Late preterm infants are infants born at a gestational age between 34+0⁄7 weeks and 36+6⁄7 weeks. They have higher morbidity and mortality rates than term infants due to their relative physiologic and metabolic immaturity, even though they are often the size and weight of some term infants. "Late preterm" has replaced "near term" to describe this group of infants, since near term incorrectly implies that these infants are "almost term" and only require routine neonatal care.
Human milk oligosaccharides (HMOs), also known as human milk glycans, are short polymers of simple sugars that can be found in high concentrations in human breast milk. Human milk oligosaccharides promote the development of the immune system, can reduce the pathogen infections and improve brain development and cognition. The HMO profile of human breast milk shapes the gut microbiota of the infant by selectively stimulating bifidobacteria and other bacteria.

Neonatal infections are infections of the neonate (newborn) acquired during prenatal development or within the first four weeks of life. Neonatal infections may be contracted by mother to child transmission, in the birth canal during childbirth, or after birth. Neonatal infections may present soon after delivery, or take several weeks to show symptoms. Some neonatal infections such as HIV, hepatitis B, and malaria do not become apparent until much later. Signs and symptoms of infection may include respiratory distress, temperature instability, irritability, poor feeding, failure to thrive, persistent crying and skin rashes.
Cracked nipple is a condition that can occur in breastfeeding women as a result of a number of possible causes. Developing a cracked nipple can result in soreness, dryness or irritation to, or bleeding of, one or both nipples during breastfeeding. The mother with a cracked nipple can have severe nipple pain when the baby is nursing. This severe pain is a disincentive for continued breastfeeding. The crack can appear as a cut across the tip of the nipple and may extend to its base. Cracked nipple can develop after the birth of the infant and is managed with pharmacological and nonpharmacological treatment.
Soy formula is a substitute for human breast milk. It is a commercial product based on the proteins found in soybeans. Soy infant formula uses processed soybeans as its source of protein, and comes in powdered or liquid form. Usually lactose-free, soy infant formula contains a different sugar. Infants who are intolerant of cows’ milk protein may also be intolerant of soy protein. It differs from human breast milk in a number of ways. Soy protein inhibits the absorption of iron. The soy-based formulas discussed by the World Health Organization reports that soy formula is fortified with iron to compensate for this effect. One naturally occurring plant-based compound found in soy-based infant formula is phytic acid. It is also a strong inhibitor of iron absorption, though it can be removed in processing. It is not known how many manufacturers of soy-based formula incorporate this practice. China and Vietnam have regulated soy-based infant formulas to include NaFeEDTA to fortify the formula and enhance the absorption of iron by the infant. When iron compounds are added to soy-based infant formula, the iron compound is encapsulated to prevent it from making the formula dark.
In breastfeeding women, low milk supply, also known as lactation insufficiency, insufficient milk syndrome, agalactia, agalactorrhea, hypogalactia or hypogalactorrhea, is the production of breast milk in daily volumes that do not fully meet the nutritional needs of her infant.
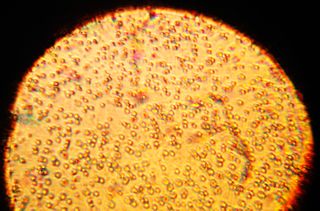
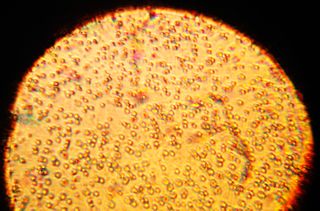
The human milk microbiota, also known as human milk probiotics (HMP), refers to the microbiota (community of microorganisms) residing in the human mammary glands and breast milk. Human breast milk has been traditionally assumed to be sterile, but more recently both microbial culture and culture-independent techniques have confirmed that human milk contains diverse communities of bacteria which are distinct from other microbial communities inhabiting the human body.
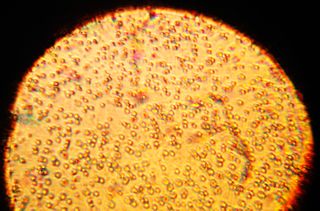
Human milk immunity is the protection provided to the immune system of an infant via the biologically active components in human milk. Human milk was previously thought to only provide passive immunity primarily through Secretory IgA, but advances in technology have led to the identification of various immune-modulating components. Human milk constituents provide nutrition and protect the immunologically naive infant as well as regulate the infant's own immune development and growth.