Phossy jaw, formally known as phosphorus necrosis of the jaw, was an occupational disease affecting those who worked with white phosphorus without proper safeguards. It was most commonly seen in workers in the matchstick industry in the 19th and early 20th centuries. It was caused by white phosphorus vapor, which destroys the bones of the jaw. Modern occupational hygiene practices have since eliminated the working conditions that caused this disease.
Hypercalcemia, also spelled hypercalcaemia, is a high calcium (Ca2+) level in the blood serum. The normal range is 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), with levels greater than 2.6 mmol/L defined as hypercalcemia. Those with a mild increase that has developed slowly typically have no symptoms. In those with greater levels or rapid onset, symptoms may include abdominal pain, bone pain, confusion, depression, weakness, kidney stones or an abnormal heart rhythm including cardiac arrest.

An osteoclast is a type of bone cell that breaks down bone tissue. This function is critical in the maintenance, repair, and remodeling of bones of the vertebral skeleton. The osteoclast disassembles and digests the composite of hydrated protein and mineral at a molecular level by secreting acid and a collagenase, a process known as bone resorption. This process also helps regulate the level of blood calcium.

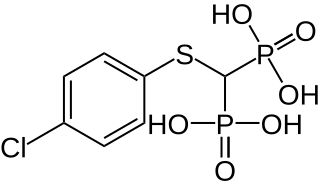
Bisphosphonates are a class of drugs that prevent the loss of bone density, used to treat osteoporosis and similar diseases. They are the most commonly prescribed drugs used to treat osteoporosis. They are called bisphosphonates because they have two phosphonate groups. They are thus also called diphosphonates.
CTX is a three-letter abbreviation with multiple meanings:

Alendronic acid, sold under the brand name Fosamax among others, is a bisphosphonate medication used to treat osteoporosis and Paget's disease of bone. It is taken by mouth. Use is often recommended together with vitamin D, calcium supplementation, and lifestyle changes.

Avascular necrosis (AVN), also called osteonecrosis or bone infarction, is death of bone tissue due to interruption of the blood supply. Early on, there may be no symptoms. Gradually joint pain may develop which may limit the ability to move. Complications may include collapse of the bone or nearby joint surface.

Osteonecrosis of the jaw (ONJ) is a severe bone disease (osteonecrosis) that affects the jaws. Various forms of ONJ have been described since 1861, and a number of causes have been suggested in the literature.

Denosumab is a human monoclonal antibody for the treatment of osteoporosis, treatment-induced bone loss, metastases to bone, and giant cell tumor of bone.
Type I collagen is the most abundant collagen of the human body. It forms large, eosinophilic fibers known as collagen fibers. It is present in scar tissue, the end product when tissue heals by repair, as well as tendons, ligaments, the endomysium of myofibrils, the organic part of bone, the dermis, the dentin, and organ capsules.

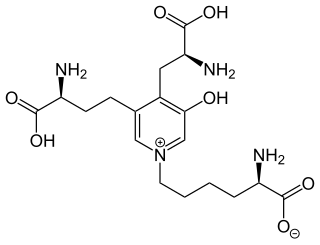
The N-terminal telopeptide (NTX), also known as amino-terminal collagen crosslinks, is the N-terminal telopeptide of fibrillar collagens such as collagen type I and type II. It is used as a biomarker to measure the rate of bone turnover. NTX can be measured in the urine (uNTX) or serum. The peptide consists of eight amino acids with the sequence YDEKSTGG.
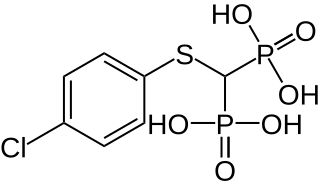
Tiludronic acid is a bisphosphonate used for treatment of Paget's disease of bone in human being medicine. It has the tradename Skelid. In veterinary medicine, tiludronic acid is used to treat navicular disease and bone spavin in horses. Its tradenames are Tildren and Equidronate. It is approved for treatment of navicular disease and distal, tarsal osteoarthritis in Europe, and was approved for treatment of navicular disease in the United States in 2014.

Medication-related osteonecrosis of the jaw is progressive death of the jawbone in a person exposed to a medication known to increase the risk of disease, in the absence of a previous radiation treatment. It may lead to surgical complication in the form of impaired wound healing following oral and maxillofacial surgery, periodontal surgery, or endodontic therapy.
Neuralgia-inducing cavitational osteonecrosis (NICO) is a controversial diagnosis whereby a putative jawbone cavitation causes chronic facial neuralgia; this is different from osteonecrosis of the jaw. In NICO the pain is said to result from the degenerating nerve ("neuralagia"). The condition is probably rare, if it does exist.
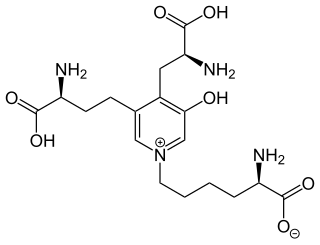
Deoxypyridinoline, also called D-Pyrilinks, Pyrilinks-D, or deoxyPYD, is one of two pyridinium cross-links that provide structural stiffness to type I collagen found in bones. It is excreted unmetabolized in urine and is a specific marker of bone resorption and osteoclastic activity. It is measured in urine tests and is used along with other bone markers such as alkaline phosphatase, osteocalcin, and N-terminal telopeptide to diagnose bone diseases such as postmenopausal osteoporosis, bone metastasis, and Paget's disease, furthermore, it has been useful in monitoring treatments that contain bone-active agents such as estrogens and bisphosphonates.
Socket preservation or alveolar ridge preservation is a procedure to reduce bone loss after tooth extraction. After tooth extraction, the jaw bone has a natural tendency to become narrow, and lose its original shape because the bone quickly resorbs, resulting in 30–60% loss in bone volume in the first six months. Bone loss, can compromise the ability to place a dental implant, or its aesthetics and functional ability.
Host modulatory therapy is an emerging treatment concept in the management of periodontitis that aims to reduce tissue destruction and stabilise or even regenerate the periodontium by modifying the host response. Historically treatment of periodontitis has been focused on reducing the bacterial challenge. However the outcomes of the conventional treatment procedures like scaling and root planning (SRP) are not always stable or predictable. Periodontal disease is seen as a balance between (1) a persisting bacterial challenge and the proinflammatory destructive events in the tissue and (2) resolution of inflammation and downregulation of destructive processes. The goal is to maximize treatment response by reducing inflammation and inhibiting destructive processes in the tissues which will result in enhanced periodontal stability after conventional periodontal treatments like SRP.
Osteomyelitis of the jaws is osteomyelitis which occurs in the bones of the jaws. Historically, osteomyelitis of the jaws was a common complication of odontogenic infection. Before the antibiotic era, it was frequently a fatal condition.
Parish P. Sedghizadeh is a clinician-scientist, and a clinical and surgical oral and maxillofacial pathologist. He is a Professor of Clinical Dentistry, and Section Chair of Diagnostic Sciences in the Division of Periodontology, Diagnostic Sciences & Dental Hygiene at the Herman Ostrow School of Dentistry, University of Southern California. He is also the Director of the Oral Pathology and Radiology Distance Learning Program at the University of Southern California.
Surgically facilitated orthodontic therapy(SFOT) is a group of orthodontic procedures; they can be broadly divided into two main categories.