Related Research Articles
The mini–mental state examination (MMSE) or Folstein test is a 30-point questionnaire that is used extensively in clinical and research settings to measure cognitive impairment. It is commonly used in medicine and allied health to screen for dementia. It is also used to estimate the severity and progression of cognitive impairment and to follow the course of cognitive changes in an individual over time; thus making it an effective way to document an individual's response to treatment. The MMSE's purpose has been not, on its own, to provide a diagnosis for any particular nosological entity.
A pain scale measures a patient's pain intensity or other features. Pain scales are a common communication tool in medical contexts, and are used in a variety of medical settings. Pain scales are a necessity to assist with better assessment of pain and patient screening. Pain measurements help determine the severity, type, and duration of the pain, and are used to make an accurate diagnosis, determine a treatment plan, and evaluate the effectiveness of treatment. Pain scales are based on trust, cartoons (behavioral), or imaginary data, and are available for neonates, infants, children, adolescents, adults, seniors, and persons whose communication is impaired. Pain assessments are often regarded as "the 5th vital sign".
Pupillometer, also spelled pupilometer, is a medical device intended to measure by reflected light the size of the pupil of the eye. In addition to measuring pupil size, current automated pupillometers may also be able to characterize pupillary light reflex. Some instruments for measuring pupillary distance (PD) are often, but incorrectly, referred to as pupilometers.
The clinical global impression (CGI) rating scales are measures of symptom severity, treatment response and the efficacy of treatments in treatment studies of patients with mental disorders. It is a brief 3-item observer-rated scale that can be used in clinical practice as well as in researches to track symptom changes. It was developed by Early Clinical Drug Evaluation Program (ECDEU) team of researchers for use in NIMH-led clinical trials that could provide clinical judgment based assessment for determining the severity of symptoms and the treatment progress. This was meant to assess the patient's functioning prior to and after initiating medication in trials which is an important part of study process. Its 3 items assess, 1) Severity of Illness (CGI-S), 2) Global Improvement (CGI-I), and 3) Efficacy Index. Many researchers, while recognizing the validity of the scale, consider it to be subjective as it requires the user of the scale to compare the subjects to typical patients in the clinician experience.
The Rancho Los Amigos Scale (RLAS), a.k.a. the Rancho Los Amigos Levels of Cognitive Functioning Scale (LOCF) or Rancho Scale, is a medical scale used to assess individuals after a closed head injury, including traumatic brain injury, based on cognitive and behavioural presentations as they emerge from coma. It is named after the Rancho Los Amigos National Rehabilitation Center, located in Downey, California, United States in Los Angeles County.
In statistics, inter-rater reliability is the degree of agreement among independent observers who rate, code, or assess the same phenomenon.
Leonard Berg was a neurologist at Washington University in St. Louis and a specialist in dementia and Alzheimer's disease. He was instrumental in the development of the Clinical Dementia Rating scale, a tool commonly used in research of these diseases.

Paratonia is the inability to relax muscles during muscle tone assessment. There are two types of paratonia: oppositional and facilitatory. Oppositional paratonia ("gegenhalten") occurs when subjects involuntarily resist passive movements, while facilitatory paratonia ("mitgehen") occurs when subjects involuntarily assist with passive movements. Both types of paratonia have been associated with cognitive impairment or mental disorders, particularly in relation to frontal lobe dysfunction. Paratonia is frequently encountered in association with dementia.
Mild cognitive impairment (MCI) is a neurocognitive disorder which involves cognitive impairments beyond those expected based on an individual's age and education but which are not significant enough to interfere with instrumental activities of daily living. MCI may occur as a transitional stage between normal aging and dementia, especially Alzheimer's disease. It includes both memory and non-memory impairments. The cause of the disorder remains unclear, as well as both its prevention and treatment, with some 50 percent of people diagnosed with it going on to develop Alzheimer's disease within five years. The diagnosis can also serve as an early indicator for other types of dementia, although MCI may remain stable or even remit.
The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) is a questionnaire that can be filled out by a relative or other supporter of an older person to determine whether that person has declined in cognitive functioning. The IQCODE is used as a screening test for dementia. If the person is found to have significant cognitive decline, then this needs to be followed up with a medical examination to determine whether dementia is present.
The California Verbal Learning Test (CVLT) is one of the most widely used neuropsychological tests in North America. As an instrument, it represents a relatively new approach to clinical psychology and the cognitive science of memory. It measures episodic verbal learning and memory, and demonstrates sensitivity to a range of clinical conditions. The test does this by attempting to link memory deficits with impaired performance on specific tasks. It assesses encoding, recall and recognition in a single modality of item presentation (auditory-verbal). The CVLT is considered to be a more sensitive measure of episodic memory than other verbal learning tests. It was designed to not only measure how much a subject learned, but also reveal strategies employed and the types of errors made. The CVLT indexes free and cued recall, serial position effects, semantic clustering, intrusions, interference and recognition. Delis et al. (1994) released the California Verbal Learning Test for Children (CVLT-C). The California Verbal Learning Test-II (CVLT-II) is an updated version of the original CVLT, which has been standardized and provides normative data.
The CDR system is a computerized battery of cognitive tests designed in the late 1970s by Professor Keith Wesnes at the University of Reading in Berkshire, England, for repeated testing in clinical trials. Task stimuli are presented in a laptop computer and participants respond via 'YES' and 'NO' buttons on a two-button response box, which records both the accuracy and reaction time.
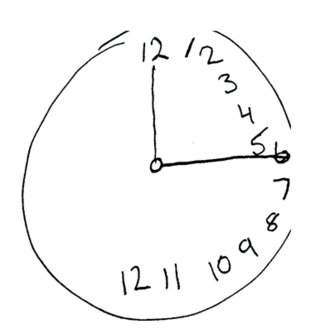
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.
The Luria–Nebraska Neuropsychological Battery (LNNB) is a standardized test that identifies neuropsychological deficiencies by measuring functioning on fourteen scales. It evaluates learning, experience, and cognitive skills. The test was created by Charles Golden in 1981 and based on previous work by Alexander Luria that emphasizes a qualitative instead of quantitative approach. The original, adult version is for use with ages fifteen and over, while the Luria–Nebraska Neuropsychological Battery for Children (LNNB-C) can be used with ages eight to twelve; both tests take two to three hours to administer. The LNNB has 269 items divided among fourteen scales, which are motor, rhythm, tactile, visual, receptive speech, expressive speech, writing, reading, arithmetic, memory, intellectual processes, pathognomonic, left hemisphere, and right hemisphere. The test is graded on scales that are correlated to regions of the brain to help identify which region may be damaged. The Luria–Nebraska has been found to be reliable and valid; it is comparable in this sense to other neuropsychological tests in its ability to differentiate between brain damage and mental illness. The test is used to diagnose and determine the nature of cognitive impairment, including the location of the brain damage, to understand the patient's brain structure and abilities, to pinpoint causes of behavior, and to help plan treatment.
Pupillometry, the measurement of pupil size and reactivity, is a key part of the clinical neurological exam for patients with a wide variety of neurological injuries. It is also used in psychology.
The Child Mania Rating Scales (CMRS) is a 21-item diagnostic screening measure designed to identify symptoms of mania in children and adolescents aged 9–17 using diagnostic criteria from the DSM-IV, developed by Pavuluri and colleagues. There is also a 10-item short form. The measure assesses the child's mood and behavior symptoms, asking parents or teachers to rate how often the symptoms have caused a problem for the youth in the past month. Clinical studies have found the CMRS to be reliable and valid when completed by parents in the assessment of children's bipolar symptoms. The CMRS also can differentiate cases of pediatric bipolar disorder from those with ADHD or no disorder, as well as delineating bipolar subtypes. A meta-analysis comparing the different rating scales available found that the CMRS was one of the best performing scales in terms of telling cases with bipolar disorder apart from other clinical diagnoses. The CMRS has also been found to provide a reliable and valid assessment of symptoms longitudinally over the course of treatment. The combination of showing good reliability and validity across multiple samples and clinical settings, along with being free and brief to score, make the CMRS a promising tool, especially since most other checklists available for youths do not assess manic symptoms.
The Virtual Reality Functional Capacity Assessment Tool (VRFCAT) is a computerized measure that was developed to be a reliable, valid, and sensitive measure of functional capacity, with the potential to demonstrate real-world functional improvements associated with cognitive change. The VRFCAT presents participants with a realistic simulated environment to recreate routine activities of daily living. The VRFCAT was developed by VeraSci under National Institute of Mental Health (NIMH) Small Business Innovation Research (SBIR) phase 1 and phase 2 grants.
See also: University of California, San Diego Performance-Based Skills Assessment
Clinicians routinely check the pupils of critically injured and ill patients to monitor neurological status. However, manual pupil measurements have been shown to be subjective, inaccurate, and not repeatable or consistent. Automated assessment of the pupillary light reflex has emerged as an objective means of measuring pupillary reactivity across a range of neurological diseases, including stroke, traumatic brain injury and edema, tumoral herniation syndromes, and sports or war injuries. Automated pupillometers are used to assess an array of objective pupillary variables including size, constriction velocity, latency, and dilation velocity, which are normalized and standardized to compute an indexed score such as the Neurological Pupil index (NPi).
The Tourette's Disorder Scale (TODS) is a psychological measure used to assess tics and co-occurring conditions in Tourette syndrome, a disease characterised by simple and complex motor and vocal tics and a wide range of behavioural and emotional symptoms. There are two versions of TODS (TODS-CR and TODS-PR), each being a 15-item scale that helps clinicians evaluate the severity of various symptoms associated with tics, inattention, hyperactivity, obsessions, compulsions, aggression and emotions.
References
- ↑ Br J Psychiatry. 1982 Jun;140:566-72. A new clinical scale for the staging of dementia. Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL.
- ↑ "Clinical Dementia Rating Assignment".
- ↑ Utility of the Clinical Dementia Rating in Asian Populations - Lim et al. 5 (1): 61 - Clinical Medicine & Research
- ↑ Rockwood, K.; Strang, D.; MacKnight, C.; Downer, R.; Morris, J. C. (2000). "Interrater reliability of the Clinical Dementia Rating in a multicenter trial". Journal of the American Geriatrics Society. 48 (5): 558–9. doi:10.1111/j.1532-5415.2000.tb05004.x. PMID 10811551. S2CID 31522657.
- ↑ Nyunt, Ma Shwe Zin; Chong, Mei Sian; Lim, Wee Shiong; Lee, Tih Shih; Yap, Philip; Ng, Tze Pin (2013-10-29). "Reliability and Validity of the Clinical Dementia Rating for Community-Living Elderly Subjects without an Informant". Dementia and Geriatric Cognitive Disorders Extra. 3 (1): 407–416. doi:10.1159/000355122. ISSN 1664-5464. PMC 3843919 . PMID 24348502.
- ↑ Morris, J. C.; Ernesto, C.; Schafer, K.; Coats, M.; Leon, S.; Sano, M.; Thal, L. J.; Woodbury, P. (1997). "Clinical Dementia Rating training and reliability in multicenter studies". Neurology. 48 (6): 1508–1510. doi:10.1212/WNL.48.6.1508. PMID 9191756. S2CID 41691732.