Related Research Articles

Alcoholism is, broadly, any drinking of alcohol that results in significant mental or physical health problems. Because there is disagreement on the definition of the word alcoholism, it is not a recognized diagnostic entity, and the use of alcoholism terminology is discouraged due to its heavily stigmatized connotations. Predominant diagnostic classifications are alcohol use disorder (DSM-5) or alcohol dependence (ICD-11); these are defined in their respective sources.

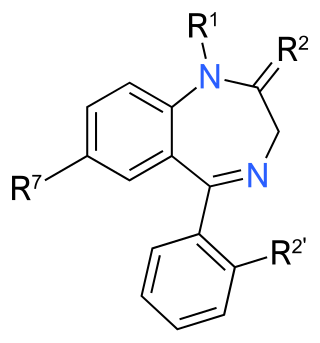
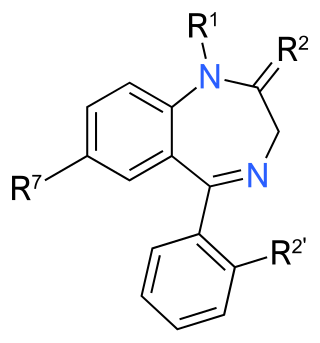
Benzodiazepines, sometimes called "benzos", are a class of depressant drugs whose core chemical structure is the fusion of a benzene ring and a diazepine ring. They are prescribed to treat conditions such as anxiety disorders, insomnia, and seizures. The first benzodiazepine, chlordiazepoxide (Librium), was discovered accidentally by Leo Sternbach in 1955 and was made available in 1960 by Hoffmann–La Roche, who soon followed with diazepam (Valium) in 1963. By 1977, benzodiazepines were the most prescribed medications globally; the introduction of selective serotonin reuptake inhibitors (SSRIs), among other factors, decreased rates of prescription, but they remain frequently used worldwide.

Diazepam, first marketed as Valium, is a medicine of the benzodiazepine family that acts as an anxiolytic. It is commonly used to treat a range of conditions, including anxiety, seizures, alcohol withdrawal syndrome, muscle spasms, insomnia, and restless legs syndrome. It may also be used to cause memory loss during certain medical procedures. It can be taken by mouth, inserted into the rectum, injected into muscle, injected into a vein or used as a nasal spray. When given into a vein, effects begin in one to five minutes and last up to an hour. By mouth, effects begin after 15 to 60 minutes.
Physical dependence is a physical condition caused by chronic use of a tolerance-forming drug, in which abrupt or gradual drug withdrawal causes unpleasant physical symptoms. Physical dependence can develop from low-dose therapeutic use of certain medications such as benzodiazepines, opioids, antiepileptics and antidepressants, as well as the recreational misuse of drugs such as alcohol, opioids and benzodiazepines. The higher the dose used, the greater the duration of use, and the earlier age use began are predictive of worsened physical dependence and thus more severe withdrawal syndromes. Acute withdrawal syndromes can last days, weeks or months. Protracted withdrawal syndrome, also known as post-acute-withdrawal syndrome or "PAWS", is a low-grade continuation of some of the symptoms of acute withdrawal, typically in a remitting-relapsing pattern, often resulting in relapse and prolonged disability of a degree to preclude the possibility of lawful employment. Protracted withdrawal syndrome can last for months, years, or depending on individual factors, indefinitely. Protracted withdrawal syndrome is noted to be most often caused by benzodiazepines. To dispel the popular misassociation with addiction, physical dependence to medications is sometimes compared to dependence on insulin by persons with diabetes.

Clorazepate, sold under the brand name Tranxene among others, is a benzodiazepine medication. It possesses anxiolytic, anticonvulsant, sedative, hypnotic, and skeletal muscle relaxant properties. Clorazepate is an unusually long-lasting benzodiazepine and serves as a majoritive prodrug for the equally long-lasting desmethyldiazepam, which is rapidly produced as an active metabolite. Desmethyldiazepam is responsible for most of the therapeutic effects of clorazepate.

Acamprosate, sold under the brand name Campral, is a medication used along with counselling to treat alcohol use disorder.

The Alcohol Use Disorders Identification Test (AUDIT) is a ten-item questionnaire approved by the World Health Organization to screen patients for hazardous (risky) and harmful alcohol consumption. It was developed from a WHO multi-country collaborative study, the items being selected for the AUDIT being the best performing of approximately 150 items including in the original survey. It is widely used as a summary measure of alcohol use and related problems. It has application in primary health care, medical clinics, and hospital units and performs well in these settings. Using different cut-off points, it can also screen for Alcohol Use Disorder (DSM-5) and Alcohol Dependence. Guidelines for the use of the AUDIT have been published by WHO and are available in several languages. It has become a widely used instrument and has been translated into approximately fifty languages.

Benzodiazepine withdrawal syndrome, often abbreviated to benzo withdrawal or BZD withdrawal, is the cluster of signs and symptoms that may emerge when a person who has been taking benzodiazepines as prescribed develops a physical dependence on them and then reduces the dose or stops taking them without a safe taper schedule.

Alcohol detoxification is the abrupt cessation of alcohol intake in individuals that have alcohol dependence. This process is often coupled with substitution of drugs that have effects similar to the effects of alcohol in order to prevent alcohol withdrawal. When withdrawal does occur, it results in symptoms of varying severity.
Post-acute withdrawal syndrome (PAWS) is a hypothesized set of persistent impairments that occur after withdrawal from alcohol, opiates, benzodiazepines, antidepressants, and other substances. Infants born to mothers who used substances of dependence during pregnancy may also experience a post-acute withdrawal syndrome. While post-acute withdrawal syndrome has been reported by those in the recovery community, there have been few scientific studies supporting its existence outside of protracted benzodiazepine withdrawal. Because of this, the disorder is not recognized by the Diagnostic and Statistical Manual of Mental Disorders or major medical associations.

Alcoholic hallucinosis is a complication of alcohol misuse in people with alcohol use disorder. It can occur during acute intoxication or withdrawal with the potential of having delirium tremens. Alcohol hallucinosis is a rather uncommon alcohol-induced psychotic disorder almost exclusively seen in chronic alcoholics who have many consecutive years of severe and heavy drinking during their lifetime. Alcoholic hallucinosis develops about 12 to 24 hours after the heavy drinking stops suddenly, and can last for days. It involves auditory and visual hallucinations, most commonly accusatory or threatening voices. The risk of developing alcoholic hallucinosis is increased by long-term heavy alcohol abuse and the use of other drugs. Descriptions of the condition date back to at least 1907.

Alcohol withdrawal syndrome (AWS) is a set of symptoms that can occur following a reduction in alcohol use after a period of excessive use. Symptoms typically include anxiety, shakiness, sweating, vomiting, fast heart rate, and a mild fever. More severe symptoms may include seizures, and delirium tremens (DTs) which can be fatal in untreated patients. Symptoms typically begin around six hours following the last drink, are worst at 24 to 72 hours, and improve by seven days.

Benzodiazepine dependence defines a situation in which one has developed one or more of either tolerance, withdrawal symptoms, drug seeking behaviors, such as continued use despite harmful effects, and maladaptive pattern of substance use, according to the DSM-IV. In the case of benzodiazepine dependence, however, the continued use seems to be associated with the avoidance of unpleasant withdrawal reaction rather than from the pleasurable effects of the drug. Benzodiazepine dependence develops with long-term use, even at low therapeutic doses, without the described dependence behavior.

Benzodiazepine overdose describes the ingestion of one of the drugs in the benzodiazepine class in quantities greater than are recommended or generally practiced. The most common symptoms of overdose include central nervous system (CNS) depression, impaired balance, ataxia, and slurred speech. Severe symptoms include coma and respiratory depression. Supportive care is the mainstay of treatment of benzodiazepine overdose. There is an antidote, flumazenil, but its use is controversial.
The effects of long-term benzodiazepine use include drug dependence and neurotoxicity as well as the possibility of adverse effects on cognitive function, physical health, and mental health. Long-term use is sometimes described as use not shorter than three months. Benzodiazepines are generally effective when used therapeutically in the short term, but even then the risk of dependency can be significantly high. There are significant physical, mental and social risks associated with the long-term use of benzodiazepines. Although anxiety can temporarily increase as a withdrawal symptom, there is evidence that a reduction or withdrawal from benzodiazepines can lead in the long run to a reduction of anxiety symptoms. Due to these increasing physical and mental symptoms from long-term use of benzodiazepines, slow withdrawal is recommended for long-term users. Not everyone, however, experiences problems with long-term use.
Benzodiazepine use disorder (BUD), also called misuse or abuse, is the use of benzodiazepines without a prescription, often for recreational purposes, which poses risks of dependence, withdrawal and other long-term effects. Benzodiazepines are one of the more common prescription drugs used recreationally. When used recreationally benzodiazepines are usually administered orally but sometimes they are taken intranasally or intravenously. Recreational use produces effects similar to alcohol intoxication.

Substance use disorder (SUD) is the persistent use of drugs despite substantial harm and adverse consequences as a result of their use. Substance use disorders are characterized by an array of mental/emotional, physical, and behavioral problems such as chronic guilt; an inability to reduce or stop consuming the substance(s) despite repeated attempts; operating vehicles while intoxicated; and physiological withdrawal symptoms. Drug classes that are commonly involved in SUD include: alcohol (alcoholism); cannabis; opioids; stimulants such as nicotine, cocaine and amphetamines; benzodiazepines; barbiturates; and other or unknown substances.
Neonatal withdrawal or neonatal abstinence syndrome (NAS) or neonatal opioid withdrawal syndrome (NOWS) is a withdrawal syndrome of infants after birth caused by in utero exposure to drugs of dependence, most commonly opioids. Common signs and symptoms include tremors, irritability, vomiting, diarrhea, and fever. NAS is primarily diagnosed with a detailed medication history and scoring systems. First-line treatment should begin with non-medication interventions to support neonate growth, though medication interventions may be used in certain situations.

Prescription drug addiction is the chronic, repeated use of a prescription drug in ways other than prescribed for, including using someone else’s prescription. A prescription drug is a pharmaceutical drug that may not be dispensed without a legal medical prescription. Drugs in this category are supervised due to their potential for misuse and Substance use disorder. The classes of medications most commonly abused are opioids, central nervous system (CNS) depressants and central nervous stimulants. In particular, prescription opioid is most commonly abused in the form of prescription analgesics.
Drug liking is a measure of the pleasurable (hedonic) experience when a person consumes drugs. It is commonly used to study the misuse liability of drugs. Drug liking is often measured using unipolar and bipolar visual analogue scales (VAS), such as the Drug Liking VAS, the High VAS, the Take Drug Again (TDA) VAS, and the Overall Drug Liking (ODL) VAS. There is a dissociation of drug liking from drug wanting. Drugs that increase scores on drug-liking measures include amphetamines, cocaine, methylphenidate, MDMA, opioids, benzodiazepines, Z-drugs, barbiturates, alcohol, nicotine, and caffeine (limitedly), among others.
References
- ↑ Sullivan, JT; Sykora, K; Schneiderman, J; Naranjo, CA; Sellers, EM (November 1989). "Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar)". British Journal of Addiction. 84 (11): 1353–7. CiteSeerX 10.1.1.489.341 . doi:10.1111/j.1360-0443.1989.tb00737.x. PMID 2597811.
- ↑ Saitz, R; Mayo-Smith, MF; Roberts, MS; Redmond, HA; Bernard, DR; Calkins, DR (17 August 1994). "Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial". JAMA. 272 (7): 519–23. doi:10.1001/jama.272.7.519. PMID 8046805.
- 1 2 Mayo-Smith, MF (9 July 1997). "Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal". JAMA. 278 (2): 144–51. doi:10.1001/jama.278.2.144. PMID 9214531.
- ↑ Sullivan, J. T.; Sykora, K.; Schneiderman, J.; Naranjo, C. A.; Sellers, E. M. (1989). "Assessment of alcohol withdrawal: The revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar)". British Journal of Addiction. 84 (11): 1353–7. doi:10.1111/j.1360-0443.1989.tb00737.x. PMID 2597811.
- ↑ Saitz M, Mayo-Smith MF, Redmond HA, Bernard DR, Calkins DR. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA 1994;272:519-23.
- ↑ Reoux, Joseph P.; Malte, Carol A.; Kivlahan, Daniel R.; Saxon, Andrew J. (20 September 2002). "The Alcohol Use Disorders Identification Test (AUDIT) Predicts Alcohol Withdrawal Symptoms During Inpatient Detoxification". Journal of Addictive Diseases. 21 (4): 81–91. doi:10.1300/J069v21n04_08. PMID 12296504. S2CID 34289594.
- ↑ Williams, Kendal; Mitchell, Matthew (6 November 2013). "Inpatient Alcohol Withdrawal: Time to Prevent the Preventable?". Journal of General Internal Medicine. 29 (1): 7–9. doi:10.1007/s11606-013-2642-7. PMC 3889962 . PMID 24197633.