A genetic disorder is a health problem caused by one or more abnormalities in the genome. It can be caused by a mutation in a single gene (monogenic) or multiple genes (polygenic) or by a chromosomal abnormality. Although polygenic disorders are the most common, the term is mostly used when discussing disorders with a single genetic cause, either in a gene or chromosome. The mutation responsible can occur spontaneously before embryonic development, or it can be inherited from two parents who are carriers of a faulty gene or from a parent with the disorder. When the genetic disorder is inherited from one or both parents, it is also classified as a hereditary disease. Some disorders are caused by a mutation on the X chromosome and have X-linked inheritance. Very few disorders are inherited on the Y chromosome or mitochondrial DNA.

Hearing loss is a partial or total inability to hear. Hearing loss may be present at birth or acquired at any time afterwards. Hearing loss may occur in one or both ears. In children, hearing problems can affect the ability to acquire spoken language, and in adults it can create difficulties with social interaction and at work. Hearing loss can be temporary or permanent. Hearing loss related to age usually affects both ears and is due to cochlear hair cell loss. In some people, particularly older people, hearing loss can result in loneliness.
This is a glossary of medical terms related to communication disorders which are psychological or medical conditions that could have the potential to affect the ways in which individuals can hear, listen, understand, speak and respond to others.

A cochlear implant (CI) is a surgically implanted neuroprosthesis that provides a person who has moderate-to-profound sensorineural hearing loss with sound perception. With the help of therapy, cochlear implants may allow for improved speech understanding in both quiet and noisy environments. A CI bypasses acoustic hearing by direct electrical stimulation of the auditory nerve. Through everyday listening and auditory training, cochlear implants allow both children and adults to learn to interpret those signals as speech and sound.

Audiology is a branch of science that studies hearing, balance, and related disorders. Audiologists treat those with hearing loss and proactively prevent related damage. By employing various testing strategies, audiologists aim to determine whether someone has normal sensitivity to sounds. If hearing loss is identified, audiologists determine which portions of hearing are affected, to what degree, and where the lesion causing the hearing loss is found. If an audiologist determines that a hearing loss or vestibular abnormality is present, they will provide recommendations for interventions or rehabilitation.

Sensorineural hearing loss (SNHL) is a type of hearing loss in which the root cause lies in the inner ear, sensory organ, or the vestibulocochlear nerve. SNHL accounts for about 90% of reported hearing loss. SNHL is usually permanent and can be mild, moderate, severe, profound, or total. Various other descriptors can be used depending on the shape of the audiogram, such as high frequency, low frequency, U-shaped, notched, peaked, or flat.
Auditory neuropathy (AN) is a hearing disorder in which the outer hair cells of the cochlea are present and functional, but sound information is not transmitted sufficiently by the auditory nerve to the brain. The cause may be several dysfunctions of the inner hair cells of the cochlea or spiral ganglion neuron levels. Hearing loss with AN can range from normal hearing sensitivity to profound hearing loss.
Post-lingual deafness is a deafness which develops after the acquisition of speech and language, usually after the age of six.

Microtia is a congenital deformity where the auricle is underdeveloped. A completely undeveloped pinna is referred to as anotia. Because microtia and anotia have the same origin, it can be referred to as microtia-anotia. Microtia can be unilateral or bilateral. Microtia occurs in 1 out of about 8,000–10,000 births. In unilateral microtia, the right ear is most commonly affected. It may occur as a complication of taking Accutane (isotretinoin) during pregnancy.

CHARGE syndrome is a rare syndrome caused by a genetic disorder. First described in 1979, the acronym "CHARGE" came into use for newborn children with the congenital features of coloboma of the eye, heart defects, atresia of the nasal choanae, restricted growth and/or development, genital and/or urinary abnormalities, and ear abnormalities and deafness. These features are no longer used in making a diagnosis of CHARGE syndrome, but the name remains. About two thirds of cases are due to a CHD7 mutation. CHARGE syndrome occurs only in 0.1–1.2 per 10,000 live births; as of 2009, it was the leading cause of congenital deafblindness in the US.
Nonsyndromic deafness is hearing loss that is not associated with other signs and symptoms. In contrast, syndromic deafness involves hearing loss that occurs with abnormalities in other parts of the body. Nonsyndromic deafness constitutes 75% of all hearing loss cases, and an estimated 100 genes are thought to be linked to this condition. About 80% are linked to autosomal recessive inheritance, 15% to autosomal dominant inheritance, 1-3% through the X chromosome, and 0.5-1% are associated with mitochondrial inheritance.

Branchio-oto-renal syndrome (BOR) is an autosomal dominant genetic disorder involving the kidneys, ears, and neck. It is also known as Melnick-Fraser syndrome.

Nager acrofacial dysostosis, also known as Nager syndrome, is a genetic disorder which displays several or all of the following characteristics: underdevelopment of the cheek and jaw area, down-sloping of the opening of the eyes, lack or absence of the lower eyelashes, kidney or stomach reflux, hammer toes, shortened soft palate, lack of development of the internal and external ear, possible cleft palate, underdevelopment or absence of the thumb, hearing loss and shortened forearms, as well as poor movement in the elbow, and may be characterized by accessory tragi. Occasionally, affected individuals develop vertebral anomalies such as scoliosis.

Large vestibular aqueduct is a structural deformity of the inner ear. Enlargement of this duct is one of the most common inner ear deformities and is commonly associated with hearing loss during childhood. The term was first discovered in 1791 by Mondini when he was completing a temporal bone dissection. It was then defined by Valvassori and Clemis as a vestibular aqueduct that is greater than or equal to 2.0 mm at the operculum and/or greater than or equal to 1.0 mm at the midpoint. Some use the term enlarged vestibular aqueduct syndrome, but this is felt by others to be erroneous as it is a clinical finding which can occur in several syndromes.
Prelingual deafness refers to deafness that occurs before learning speech or language. Speech and language typically begin to develop very early with infants saying their first words by age one. Therefore, prelingual deafness is considered to occur before the age of one, where a baby is either born deaf or loses hearing before the age of one. This hearing loss may occur for a variety of reasons and impacts cognitive, social, and language development.
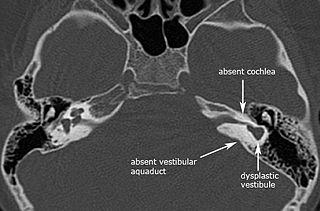
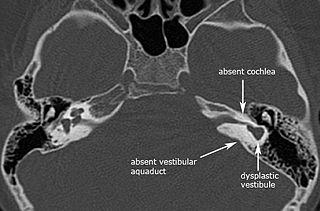
Michel aplasia, also known as complete labyrinthine aplasia (CLA), is a congenital abnormality of the inner ear. It is characterized by the bilateral absence of differentiated inner ear structures and results in complete deafness (anacusis). Michel aplasia should not be confused with michel dysplasia. It may affect one or both ears.
Language deprivation in deaf and hard-of-hearing children is a delay in language development that occurs when sufficient exposure to language, spoken or signed, is not provided in the first few years of a deaf or hard of hearing child's life, often called the critical or sensitive period. Early intervention, parental involvement, and other resources all work to prevent language deprivation. Children who experience limited access to language—spoken or signed—may not develop the necessary skills to successfully assimilate into the academic learning environment. There are various educational approaches for teaching deaf and hard of hearing individuals. Decisions about language instruction is dependent upon a number of factors including extent of hearing loss, availability of programs, and family dynamics.
Language exposure for children is the act of making language readily available and accessible during the critical period for language acquisition. Deaf and hard of hearing children, when compared to their hearing peers, tend to face more hardships when it comes to ensuring that they will receive accessible language during their formative years. Therefore, deaf and hard of hearing children are more likely to have language deprivation which causes cognitive delays. Early exposure to language enables the brain to fully develop cognitive and linguistic skills as well as language fluency and comprehension later in life. Hearing parents of deaf and hard of hearing children face unique barriers when it comes to providing language exposure for their children. Yet, there is a lot of research, advice, and services available to those parents of deaf and hard of hearing children who may not know how to start in providing language.

Achalasia microcephaly syndrome is a rare condition whereby achalasia in the oesophagus manifests alongside microcephaly and intellectual disability. This is a rare constellation of symptoms with a predicted familial trend.
Deaf and hard of hearing individuals with additional disabilities are referred to as "Deaf Plus" or "Deaf+". Deaf children with one or more co-occurring disabilities could also be referred to as hearing loss plus additional disabilities or Deafness and Diversity (D.A.D.). About 40–50% of deaf children experience one or more additional disabilities, with learning disabilities, intellectual disabilities, autism spectrum disorder (ASD), and visual impairments being the four most concomitant disabilities. Approximately 7–8% of deaf children have a learning disability. Deaf plus individuals utilize various language modalities to best fit their communication needs.