Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by symptoms of inattention, hyperactivity, impulsivity and emotional dysregulation that are excessive and pervasive, impairing in multiple contexts, and developmentally-inappropriate. ADHD symptoms arise from executive dysfunction.

Conduct disorder (CD) is a mental disorder diagnosed in childhood or adolescence that presents itself through a repetitive and persistent pattern of behavior that includes theft, lies, physical violence that may lead to destruction, and reckless breaking of rules, in which the basic rights of others or major age-appropriate norms are violated. These behaviors are often referred to as "antisocial behaviors", and is often seen as the precursor to antisocial personality disorder; however, the latter, by definition, cannot be diagnosed until the individual is 18 years old. Conduct disorder may result from parental rejection and neglect and in such cases can be treated with family therapy, as well as behavioral modifications and pharmacotherapy. It may also be caused by environmental lead exposure. Conduct disorder is estimated to affect 51.1 million people globally as of 2013.
Cognitive disengagement syndrome (CDS) is a syndrome characterized by developmentally inappropriate, impairing, and persistent levels of decoupled attentional processing from the ongoing external context and resultant hypoactivity. Symptoms often manifest in difficulties with staring, mind blanking, absent-mindedness, mental confusion and maladaptive mind-wandering alongside delayed, sedentary or slow motor movements. To scientists in the field, it has reached the threshold of evidence and recognition as a distinct syndrome.
Oppositional defiant disorder (ODD) is listed in the DSM-5 under Disruptive, impulse-control, and conduct disorders and defined as "a pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness." This behavior is usually targeted toward peers, parents, teachers, and other authority figures, including law enforcement officials. Unlike conduct disorder (CD), those with ODD do not generally show patterns of aggression towards random people, violence against animals, destruction of property, theft, or deceit. One-half of children with ODD also fulfill the diagnostic criteria for ADHD.
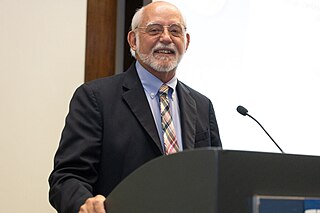
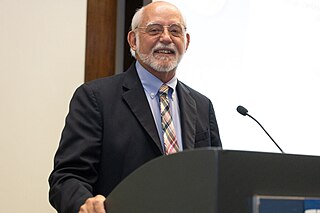
Russell Alan BarkleyFAPA is a retired American clinical neuropsychologist who was a clinical professor of psychiatry at the VCU Medical Center until 2022 and president of Division 12 of the American Psychological Association (APA) and of the International Society for Research in Child and Adolescent Psychopathology. Involved in research since 1973 and a licensed psychologist since 1977, he is an expert on attention-deficit hyperactivity disorder (ADHD) and has devoted much of his scientific career to studying ADHD and related fields like childhood defiance. He proposed the renaming of sluggish cognitive tempo (SCT) to cognitive disengagement syndrome (CDS).

Despite the scientifically well-established nature of attention deficit hyperactivity disorder (ADHD), its diagnosis, and its treatment, each of these has been controversial since the 1970s. The controversies involve clinicians, teachers, policymakers, parents, and the media. Positions range from the view that ADHD is within the normal range of behavior to the hypothesis that ADHD is a genetic condition. Other areas of controversy include the use of stimulant medications in children, the method of diagnosis, and the possibility of overdiagnosis. In 2009, the National Institute for Health and Care Excellence, while acknowledging the controversy, stated that the current treatments and methods of diagnosis are based on the dominant view of the academic literature.
Attention deficit hyperactivity disorder management options are evidence-based practices with established treatment efficacy for ADHD. Approaches that have been evaluated in the management of ADHD symptoms include FDA-approved pharmacologic treatment and other pharmaceutical agents, psychological or behavioral approaches, combined pharmacological and behavioral approaches, cognitive training, neurofeedback, neurostimulation, physical exercise, nutrition and supplements, integrative medicine, parent support, and school interventions. Based on two 2024 systematic reviews of the literature, FDA-approved medications and to a lesser extent psychosocial interventions have been shown to improve core ADHD symptoms compared to control groups.
The Strengths and Difficulties Questionnaire (SDQ) is a screening questionnaire for emotional and behavioral problems in children and adolescents ages 2 through 17 years old, developed by child psychiatrist Robert N. Goodman in the United Kingdom. The questionnaire is quite brief with 25 questions and, depending on the version, a few questions about how the child is affected by the difficulties in their everyday life. Versions of it are available for use for no fee. The combination of its brevity and noncommercial distribution have made it popular among clinicians and researchers. Overall, the SDQ has proved to have satisfactory construct and concurrent validity across a wide range of settings and samples. It is considered a good general screening measure for attention problems, although the sensitivity and specificity are not both over .80 at any single cut score, so it should not be used by itself as the basis for a diagnosis of attention-deficit/hyperactivity disorder.
The Pediatric Attention Disorders Diagnostic Screener (PADDS), created by Dr. Thomas K. Pedigo and Kenneth L. Pedigo, is a suite of computer administered neuropsychological tests of attention and executive functioning. The PADDS is used in the diagnosis of attention deficit hyperactivity disorder (ADHD) in children between the ages of 6 and 12 years. The PADDS software program represents a multi-dimensional, evidence-based approach to ADHD assessment, consisting of the Computer Administered Diagnostic Interview (CADI), the Swanson, Nolan, and Pelham—IV (SNAP-IV) Parent and Teacher rating scales, and the three computer-administered objective measures of the Target Tests of Executive Functioning (TTEF). It calculates a diagnostic likelihood ratio, where each data source is allowed to contribute to (or detract from) the prediction of the diagnosis, as well as normalized relative standard scores, t-scores, z-scores, and percentile ranks for comparison to the non-clinical reference group.
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by difficulty focusing attention, hyperactivity, and impulsive behavior. Treatments generally involve behavioral therapy and/or medications. ADHD is estimated to affect about 6 to 7 percent of people aged 18 and under when diagnosed via the DSM-IV criteria. However, these estimates may be inaccurate as females tend to have fewer symptoms, as identified in the DSM-IV, and thus tend to be under-diagnosed due to these sex differences in predicting ADHD. When diagnosed via the ICD-10 criteria, hyperkinetic disorder gives rates between 1 and 2 percent in this age group.
The Swanson, Nolan and Pelham Teacher and Parent Rating Scale (SNAP), developed by James Swanson, Edith Nolan and William Pelham, is a 90-question self-report inventory designed to measure attention deficit hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) symptoms in children and young adults.
The Vanderbilt ADHD Diagnostic Rating Scale (VADRS) is a psychological assessment tool for attention deficit hyperactivity disorder (ADHD) symptoms and their effects on behavior and academic performance in children ages 6–12. This measure was developed by Mark L Wolraich at the Oklahoma Health Sciences Center and includes items related to oppositional defiant disorder, conduct disorder, anxiety, and depression, disorders often comorbid with ADHD.
The ADHD Rating Scale (ADHD-RS) is a parent-report or teacher-report inventory created by George J. DuPaul, Thomas J. Power, Arthur D. Anastopoulos, and Robert Reid consisting of 18–90 questions regarding a child's behavior over the past 6 months. The ADHD Rating Scale is used to aid in the diagnosis of attention deficit hyperactivity disorder (ADHD) in children ranging from ages 5–17.
The Yale Global Tic Severity Scale (YGTSS) is a psychological measure designed to assess the severity and frequency of symptoms of disorders such as tic disorder, Tourette syndrome, and obsessive-compulsive disorder, in children and adolescents between ages 6 and 17.
The Screen for Child Anxiety Related Emotional Disorders (SCARED) is a self-report screening questionnaire for anxiety disorders developed in 1997. The SCARED is intended for youth, 9–18 years old, and their parents to complete in about 10 minutes. It can discriminate between depression and anxiety, as well as among distinct anxiety disorders. The SCARED is useful for generalized anxiety disorder, social anxiety disorder, phobic disorders, and school anxiety problems. Most available self-report instruments that measure anxiety in children look at general aspects of anxiety rather than Diagnostic and Statistical Manual of Mental Disorders (DSM) categorizations. The SCARED was developed as an instrument for both children and their parents that would encompass several DSM-IV and DSM-5 categorizations of the anxiety disorders: somatic/panic, generalized anxiety, separation anxiety, social phobia, and school phobia.
The Mood Disorder Questionnaire (MDQ) is a self-report questionnaire designed to help detect bipolar disorder. It focuses on symptoms of hypomania and mania, which are the mood states that separate bipolar disorders from other types of depression and mood disorder. It has 5 main questions, and the first question has 13 parts, for a total of 17 questions. The MDQ was originally tested with adults, but it also has been studied in adolescents ages 11 years and above. It takes approximately 5–10 minutes to complete. In 2006, a parent-report version was created to allow for assessment of bipolar symptoms in children or adolescents from a caregiver perspective, with the research looking at youths as young as 5 years old. The MDQ has become one of the most widely studied and used questionnaires for bipolar disorder, and it has been translated into more than a dozen languages.
The Child Mania Rating Scales (CMRS) is a 21-item diagnostic screening measure designed to identify symptoms of mania in children and adolescents aged 9–17 using diagnostic criteria from the DSM-IV, developed by Pavuluri and colleagues. There is also a 10-item short form. The measure assesses the child's mood and behavior symptoms, asking parents or teachers to rate how often the symptoms have caused a problem for the youth in the past month. Clinical studies have found the CMRS to be reliable and valid when completed by parents in the assessment of children's bipolar symptoms. The CMRS also can differentiate cases of pediatric bipolar disorder from those with ADHD or no disorder, as well as delineating bipolar subtypes. A meta-analysis comparing the different rating scales available found that the CMRS was one of the best performing scales in terms of telling cases with bipolar disorder apart from other clinical diagnoses. The CMRS has also been found to provide a reliable and valid assessment of symptoms longitudinally over the course of treatment. The combination of showing good reliability and validity across multiple samples and clinical settings, along with being free and brief to score, make the CMRS a promising tool, especially since most other checklists available for youths do not assess manic symptoms.
The Mood and Feelings Questionnaire is a survey that measures depressive symptoms in children and young adults. It was developed by Adrian Angold and Elizabeth J. Costello in 1987, and validity data were gathered as part of the Great Smokey Mountain epidemiological study in Western North Carolina. The questionnaire consists of a variety of statements describing feelings or behaviors that may manifest as depressive symptoms in children between the ages of 6 and 17. The subject is asked to indicate how much each statement applies to their recent experiences. The Mood and Feelings Questionnaire has six versions, short and long forms of each of the following: a youth self-report, a version that a parent would complete, and a self-report version for adults. Several peer-reviewed studies have found the Mood and Feelings Questionnaire to be a reliable and valid measure of depression in children. Compared to many other depression scales for youth, it has more extensive coverage of symptoms and more age-appropriate wording and content.
The General Behavior Inventory (GBI) is a 73-question psychological self-report assessment tool designed by Richard Depue and colleagues to identify the presence and severity of manic and depressive moods in adults, as well as to assess for cyclothymia. It is one of the most widely used psychometric tests for measuring the severity of bipolar disorder and the fluctuation of symptoms over time. The GBI is intended to be administered for adult populations; however, it has been adapted into versions that allow for juvenile populations, as well as a short version that allows for it to be used as a screening test.
The Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS) is a semi-structured interview aimed at early diagnosis of affective disorders such as depression, bipolar disorder, and anxiety disorder. There are different versions of the test that have use different versions of diagnostic criteria, cover somewhat different diagnoses and use different rating scales for the items. All versions are structured to include interviews with both the child and the parents or guardians, and all use a combination of screening questions and more comprehensive modules to balance interview length and thoroughness.