Nociception is the sensory nervous system's process of encoding noxious stimuli. It deals with a series of events and processes required for an organism to receive a painful stimulus, convert it to a molecular signal, and recognize and characterize the signal in order to trigger an appropriate defense response.

Syringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. Often, syringomyelia is used as a generic term before an etiology is determined. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in loss of feeling, paralysis, weakness, and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. It may also lead to a cape-like bilateral loss of pain and temperature sensation along the upper chest and arms. Each patient experiences a different combination of symptoms. These symptoms typically vary depending on the extent and, often more critically, on the location of the syrinx within the spinal cord.

The brainstem is the posterior stalk-like part of the brain that connects the cerebrum with the spinal cord. In the human brain the brainstem is composed of the midbrain, the pons, and the medulla oblongata. The midbrain is continuous with the thalamus of the diencephalon through the tentorial notch, and sometimes the diencephalon is included in the brainstem.
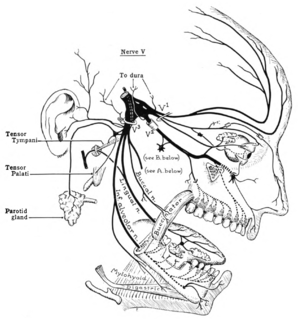
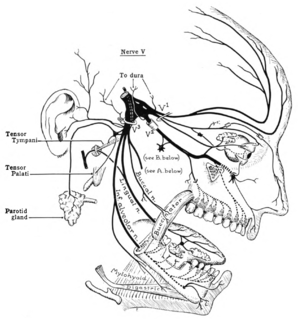
The trigeminal nerve (the fifth cranial nerve, or simply CN V) is a nerve responsible for sensation in the face and motor functions such as biting and chewing; it is the most complex of the cranial nerves. Its name ("trigeminal" = tri-, or three, and - geminus, or twin: so "three-born, triplet") derives from each of the two nerves (one on each side of the pons) having three major branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). The ophthalmic and maxillary nerves are purely sensory, whereas the mandibular nerve supplies motor as well as sensory (or "cutaneous") functions. Adding to the complexity of this nerve is that autonomic nerve fibers as well as special sensory fibers (taste) are contained within it.

The grey column refers to a somewhat ridge-shaped mass of grey matter in the spinal cord. This presents as three columns: the anterior grey column, the posterior grey column, and the lateral grey column, all of which are visible in cross-section of the spinal cord.

The pyramidal tracts include both the corticobulbar tract and the corticospinal tract. These are aggregations of efferent nerve fibers from the upper motor neurons that travel from the cerebral cortex and terminate either in the brainstem (corticobulbar) or spinal cord (corticospinal) and are involved in the control of motor functions of the body.

The spinothalamic tract is a part of the anterolateral system or the ventrolateral system, a sensory pathway to the thalamus. From the ventral posterolateral nucleus in the thalamus, sensory information is relayed upward to the somatosensory cortex of the postcentral gyrus.

The dorsal column–medial lemniscus pathway (DCML) is a sensory pathway of the central nervous system that conveys sensations of fine touch, vibration, two-point discrimination, and proprioception (position) from the skin and joints. It transmits information from the body to the primary somatosensory cortex in the postcentral gyrus of the parietal lobe of the brain. The pathway receives information from sensory receptors throughout the body, and carries this in nerve tracts in the white matter of the dorsal column of the spinal cord to the medulla, where it is continued in the medial lemniscus, on to the thalamus and relayed from there through the internal capsule and transmitted to the somatosensory cortex. The name dorsal-column medial lemniscus comes from the two structures that carry the sensory information: the dorsal columns of the spinal cord, and the medial lemniscus in the brainstem.

Medial medullary syndrome, also known as inferior alternating syndrome, hypoglossal alternating hemiplegia, lower alternating hemiplegia, or Dejerine syndrome, is a type of alternating hemiplegia characterized by a set of clinical features resulting from occlusion of the anterior spinal artery. This results in the infarction of medial part of the medulla oblongata.
Stereognosis is the ability to perceive and recognize the form of an object in the absence of visual and auditory information, by using tactile information to provide cues from texture, size, spatial properties, and temperature, etc. In humans, this sense, along with tactile spatial acuity, vibration perception, texture discrimination and proprioception, is mediated by the dorsal column-medial lemniscus pathway of the central nervous system. Stereognosis tests determine whether or not the parietal lobe of the brain is intact. Typically, these tests involved having the patient identify common objects placed in their hand without any visual cues. Stereognosis is a higher cerebral associative cortical function.

The vestibulospinal tract is a neural tract in the central nervous system. Specifically, it is a component of the extrapyramidal system and is classified as a component of the medial pathway. Like other descending motor pathways, the vestibulospinal fibers of the tract relay information from nuclei to motor neurons. The vestibular nuclei receive information through the vestibulocochlear nerve about changes in the orientation of the head. The nuclei relay motor commands through the vestibulospinal tract. The function of these motor commands is to alter muscle tone, extend, and change the position of the limbs and head with the goal of supporting posture and maintaining balance of the body and head.

The facial motor nucleus is a collection of neurons in the brainstem that belong to the facial nerve. These lower motor neurons innervate the muscles of facial expression and the stapedius.

Alpha (α) motor neurons (also called alpha motoneurons), are large, multipolar lower motor neurons of the brainstem and spinal cord. They innervate extrafusal muscle fibers of skeletal muscle and are directly responsible for initiating their contraction. Alpha motor neurons are distinct from gamma motor neurons, which innervate intrafusal muscle fibers of muscle spindles.
A syrinx is a rare, fluid-filled neuroglial cavity within the spinal cord (syringomyelia), in the brain stem (syringobulbia), or in the nerves of the elbow, usually in a young age.
Syringobulbia is a medical condition in which syrinxes, or fluid-filled cavities, affect the brainstem. The exact cause is often unknown, but may be linked to a widening of the central canal of the spinal cord. This may affect one or more cranial nerves, resulting in various kinds of facial palsies. Sensory and motor nerve pathways may be affected by interruption or compression of nerves. This disorder is associated with syringomyelia, a syrinx limited to the spinal cord. It can be diagnosed using magnetic resonance imaging. Symptoms may be treated with tricyclic antidepressants.

The posterior spinal artery arises from the vertebral artery in 25% of humans or the posterior inferior cerebellar artery in 75% of humans, adjacent to the medulla oblongata. It supplies the grey and white posterior columns of the spinal cord.

Anterior spinal artery syndrome is syndrome caused by ischemia of the anterior spinal artery, resulting in loss of function of the anterior two-thirds of the spinal cord. The region affected includes the descending corticospinal tract, ascending spinothalamic tract, and autonomic fibers. It is characterized by a corresponding loss of motor function, loss of pain and temperature sensation, and hypotension.

Brown-Séquard syndrome is caused by damage to one half of the spinal cord, i.e. hemisection of the spinal cord resulting in paralysis and loss of proprioception on the same side as the injury or lesion, and loss of pain and temperature sensation on the opposite side as the lesion. It is named after physiologist Charles-Édouard Brown-Séquard, who first described the condition in 1850.

The anterior white commissure is a bundle of nerve fibers which cross the midline of the spinal cord just anterior to the gray commissure. A delta fibers and C fibers carrying pain sensation in the spinothalamic tract contribute to this commissure, as do fibers of the anterior corticospinal tract, which carry motor signals from the primary motor cortex.

The spinal cord is a long, thin, tubular structure made up of nervous tissue, which extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column. It encloses the central canal of the spinal cord, which contains cerebrospinal fluid. The brain and spinal cord together make up the central nervous system (CNS). In humans, the spinal cord begins at the occipital bone, passing through the foramen magnum and entering the spinal canal at the beginning of the cervical vertebrae. The spinal cord extends down to between the first and second lumbar vertebrae, where it ends. The enclosing bony vertebral column protects the relatively shorter spinal cord. It is around 45 cm (18 in) long in adult men and around 43 cm (17 in) long in adult women. The diameter of the spinal cord ranges from 13 mm in the cervical and lumbar regions to 6.4 mm in the thoracic area.