Related Research Articles

The Controlled Substances Act (CSA) is the statute establishing federal U.S. drug policy under which the manufacture, importation, possession, use, and distribution of certain substances is regulated. It was passed by the 91st United States Congress as Title II of the Comprehensive Drug Abuse Prevention and Control Act of 1970 and signed into law by President Richard Nixon. The Act also served as the national implementing legislation for the Single Convention on Narcotic Drugs.

The United States Food and Drug Administration is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food safety, tobacco products, caffeine products, dietary supplements, prescription and over-the-counter pharmaceutical drugs (medications), vaccines, biopharmaceuticals, blood transfusions, medical devices, electromagnetic radiation emitting devices (ERED), cosmetics, animal foods & feed and veterinary products.

Over-the-counter (OTC) drugs are medicines sold directly to a consumer without a requirement for a prescription from a healthcare professional, as opposed to prescription drugs, which may be supplied only to consumers possessing a valid prescription. In many countries, OTC drugs are selected by a regulatory agency to ensure that they contain ingredients that are safe and effective when used without a physician's care. OTC drugs are usually regulated according to their active pharmaceutical ingredient (API) rather than final products. By regulating APIs instead of specific drug formulations, governments allow manufacturers the freedom to formulate ingredients, or combinations of ingredients, into proprietary mixtures.
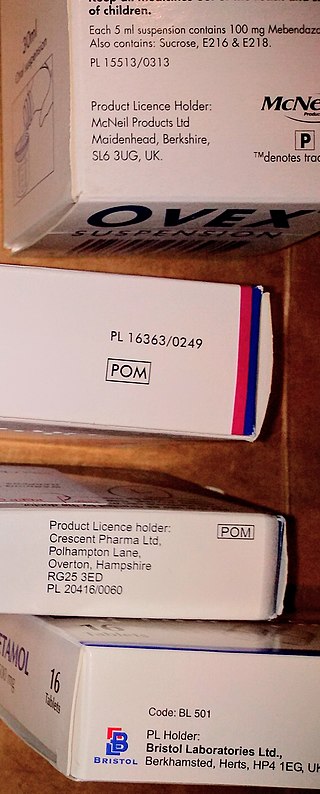
A prescription drug is a pharmaceutical drug that is permitted to be dispensed only to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.

Current good manufacturing practices (cGMP) are those conforming to the guidelines recommended by relevant agencies. Those agencies control the authorization and licensing of the manufacture and sale of food and beverages, cosmetics, pharmaceutical products, dietary supplements, and medical devices. These guidelines provide minimum requirements that a manufacturer must meet to assure that their products are consistently high in quality, from batch to batch, for their intended use. The rules that govern each industry may differ significantly; however, the main purpose of GMP is always to prevent harm from occurring to the end user. Additional tenets include ensuring the end product is free from contamination, that it is consistent in its manufacture, that its manufacture has been well documented, that personnel are well trained, and that the product has been checked for quality more than just at the end phase. GMP is typically ensured through the effective use of a quality management system (QMS).

The regulation of therapeutic goods, defined as drugs and therapeutic devices, varies by jurisdiction. In some countries, such as the United States, they are regulated at the national level by a single agency. In other jurisdictions they are regulated at the state level, or at both state and national levels by various bodies, as in Australia.

The United States Federal Food, Drug, and Cosmetic Act is a set of laws passed by the United States Congress in 1938 giving authority to the U.S. Food and Drug Administration (FDA) to oversee the safety of food, drugs, medical devices, and cosmetics. The FDA's principal representative with members of congress during its drafting was Charles W. Crawford. A principal author of this law was Royal S. Copeland, a three-term U.S. senator from New York. In 1968, the Electronic Product Radiation Control provisions were added to the FD&C. Also in that year the FDA formed the Drug Efficacy Study Implementation (DESI) to incorporate into FD&C regulations the recommendations from a National Academy of Sciences investigation of effectiveness of previously marketed drugs. The act has been amended many times, most recently to add requirements about bioterrorism preparations.

The Standard for the Uniform Scheduling of Medicines and Poisons (SUSMP), also known as the Poisons Standard for short, is an Australian legislative instrument produced by the Therapeutic Goods Administration (TGA). Before 2010, it was known as the Standard for the Uniform Scheduling of Drugs and Poisons (SUSDP). The SUSMP classifies drugs and poisons into different Schedules signifying the degree of control recommended to be exercised over their availability to the public. As of 2023, the most recent version is the Therapeutic Goods Instrument 2023.
The law in the United Kingdom on food information and labelling is multifaceted and is spread over many reforms and parliamentary acts. UK law is based on the relevant European Union rules, chiefly Regulation (EU) 1169/2011, which is implemented in the UK in the Food Information Regulations 2014, the Food Information (Wales) Regulations 2014, the Food Information (Scotland) Regulations 2014 and the Food Information Regulations 2014. Regulations apply to the labelling of goods pre-packaged for sale and to the provision of information regarding non-prepacked (loose) foods.

A package insert is a document included in the package of a medication that provides information about that drug and its use. For prescription medications, the insert is technical, providing information for medical professionals about how to prescribe the drug. Package inserts for prescription drugs often include a separate document called a "patient package insert" with information written in plain language intended for the end-user—the person who will take the drug or give the drug to another person, such as a minor. Inserts for over-the-counter medications are also written plainly.
Direct-to-consumer advertising (DTCA) refers to the marketing and advertising of pharmaceutical products directly to consumers as patients, as opposed to specifically targeting health professionals. The term is synonymous primarily with the advertising of prescription medicines via mass media platforms—most commonly on television and in magazines, but also via online platforms.
A Health and welfare trust (HAWT) or Health and welfare plan (HAWP) is a tax-free vehicle for financing a corporation's healthcare costs for their employees. They were introduced in 1986 by Canada Revenue Agency (CRA) in their interpretation bulletin entitled IT-85R2. Many companies offer this product to Canadian employers.
Electronic Prescriptions for Controlled Substances (EPCS) was originally a proposal for the DEA to revise its regulations to provide practitioners with the option of writing electronic prescriptions for controlled substances. These regulations would also permit pharmacies to receive, dispense, and archive these electronic prescriptions. These proposed regulations would be an addition to, not a replacement of, the existing rule.
Because of the uncertain nature of various alternative therapies and the wide variety of claims different practitioners make, alternative medicine has been a source of vigorous debate, even over the definition of "alternative medicine". Dietary supplements, their ingredients, safety, and claims, are a continual source of controversy. In some cases, political issues, mainstream medicine and alternative medicine all collide, such as in cases where synthetic drugs are legal but the herbal sources of the same active chemical are banned.

The Drugs and Cosmetics Act, 1940 is an act of the Parliament of India which regulates the import, manufacture and distribution of drugs in India. The primary objective of the act is to ensure that the drugs and cosmetics sold in India are safe, effective and conform to state quality standards. The related Drugs and Cosmetics Rules, 1945 contains provisions for classification of drugs under given schedules and there are guidelines for the storage, sale, display and prescription of each schedule.
Online pharmacy laws in India are still in nascent stage and there are no dedicated online pharmacy laws in India. The Information Technology Act 2000 governs some of the legal issues pertaining to online dealings but it is silent on the aspect of online pharmacy. As a result, illegal online pharmacies have been increasing in India. It has been said that, if properly regulated, online pharmacies in India could prove beneficial to various stakeholders.

The term cosmetic packaging is used for containers and secondary packaging of fragrances and cosmetic products. Cosmetic products are substances intended for human cleansing, beautifying and promoting an enhanced appearance without altering the body's structure or functions.
The distribution of medications has special drug safety and security considerations. Some drugs require cold chain management in their distribution.
Consumer Health Laws are laws that ensure that health products are safe and effective and that health professionals are competent; that government agencies enforce the laws and keep the public informed; professional, voluntary, and business organizations that serve as consumer advocates, monitor government agencies that issue safety regulations, and provide trustworthy information about health products and services; education of the consumer to permit freedom of choice based on an understanding of scientific data rather than misleading information; action by individuals to register complaints when they have been deceived, misled, overcharged, or victimized by frauds.

Drug labelling is also referred to as prescription labelling, is a written, printed or graphic matter upon any drugs or any of its container, or accompanying such a drug. Drug labels seek to identify drug contents and to state specific instructions or warnings for administration, storage and disposal. Since 1800s, legislation has been advocated to stipulate the formats of drug labelling due to the demand for an equitable trading platform, the need of identification of toxins and the awareness of public health. Variations in healthcare system, drug incidents and commercial utilization may attribute to different regional or national drug label requirements. Despite the advancement in drug labelling, medication errors are partly associated with undesirable drug label formatting.
References
- 1 2 Dr. Lily Srivastava (2010). Law & Medicine. Universal Law Publishing. pp. 216–. ISBN 978-81-7534-949-0.
- ↑ Pillay (30 November 2012). Modern Medical Toxicology. Jaypee Brothers Publishers. p. 30. ISBN 978-93-5025-965-8 . Retrieved 22 February 2015.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 "Drugs and Cosmetics Act, 1940" (PDF). Central Drugs Standard Control Organization. Archived from the original (PDF) on 31 October 2005. Retrieved 19 February 2015.
- 1 2 3 P.V. Guharaj (2003). Forensic Medicine. Orient Blackswan. p. 327. ISBN 978-81-250-2488-0 . Retrieved 20 December 2023.
- ↑ "Schedule H, Schedule X and Schedule H1 Drugs - GKToday". www.gktoday.in. Retrieved 20 December 2023.
- ↑ Dey, Sushmi (24 September 2012). "Plan to ease morphine procurement for use in pain relief". Business Standard . Retrieved 20 December 2023.
- ↑ "Modifications in Drugs and Cosmetics Act (1940) and Rules | Centre for Science and Environment" (PDF). cseindia.org. Retrieved 20 December 2023.