Related Research Articles

Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. Cognitive behavioral therapy is one of the most effective means of treatment for substance abuse and co-occurring mental health disorders. CBT focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include many issues and the treatment of many mental health conditions, including anxiety, substance use disorders, marital problems, ADHD, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.
Group psychotherapy or group therapy is a form of psychotherapy in which one or more therapists treat a small group of clients together as a group. The term can legitimately refer to any form of psychotherapy when delivered in a group format, including art therapy, cognitive behavioral therapy or interpersonal therapy, but it is usually applied to psychodynamic group therapy where the group context and group process is explicitly utilized as a mechanism of change by developing, exploring and examining interpersonal relationships within the group.

Borderline personality disorder (BPD), also known as emotionally unstable personality disorder (EUPD), is a personality disorder characterized by a long-term pattern of intense and unstable interpersonal relationships, distorted sense of self, and strong emotional reactions. Those affected often engage in self-harm and other dangerous behaviors, often due to their difficulty with returning their emotional level to a healthy or normal baseline. They may also struggle with dissociation, a feeling of emptiness, and a fear of abandonment.
Histrionic personality disorder (HPD) is defined by the American Psychiatric Association as a personality disorder characterized by a pattern of excessive attention-seeking behaviors, usually beginning in early adulthood, including inappropriate seduction and an excessive desire for approval. People diagnosed with the disorder are said to be lively, dramatic, vivacious, enthusiastic, extroverted and flirtatious.
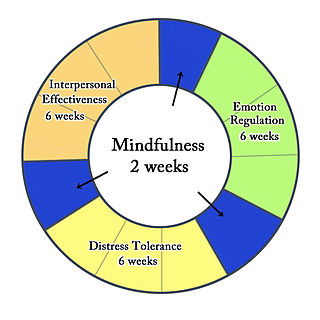
Dialectical behavior therapy (DBT) is an evidence-based psychotherapy that began with efforts to treat personality disorders and interpersonal conflicts. Evidence suggests that DBT can be useful in treating mood disorders and suicidal ideation as well as for changing behavioral patterns such as self-harm and substance use. DBT evolved into a process in which the therapist and client work with acceptance and change-oriented strategies and ultimately balance and synthesize them—comparable to the philosophical dialectical process of thesis and antithesis, followed by synthesis.
Cognitive restructuring (CR) is a psychotherapeutic process of learning to identify and dispute irrational or maladaptive thoughts known as cognitive distortions, such as all-or-nothing thinking (splitting), magical thinking, overgeneralization, magnification, and emotional reasoning, which are commonly associated with many mental health disorders. CR employs many strategies, such as Socratic questioning, thought recording, and guided imagery, and is used in many types of therapies, including cognitive behavioral therapy (CBT) and rational emotive behaviour therapy (REBT). A number of studies demonstrate considerable efficacy in using CR-based therapies.
Cognitive analytic therapy (CAT) is a form of psychological therapy initially developed in the United Kingdom by Anthony Ryle. This time-limited therapy was developed in the context of the UK's National Health Service with the aim of providing effective and affordable psychological treatment which could be realistically provided in a resource constrained public health system. It is distinctive due to its intensive use of reformulation, its integration of cognitive and analytic practice and its collaborative nature, involving the patient very actively in their treatment.
Psychodynamic psychotherapy and psychoanalytic psychotherapy are two categories of psychological therapies. Their main purpose is revealing the unconscious content of a client's psyche in an effort to alleviate psychic tension, which is inner conflict within the mind that was created in a situation of extreme stress or emotional hardship, often in the state of distress. The terms "psychoanalytic psychotherapy" and "psychodynamic psychotherapy" are often used interchangeably, but a distinction can be made in practice: though psychodynamic psychotherapy largely relies on psychoanalytical theory, it employs substantially shorter treatment periods than traditional psychoanalytical therapies. Psychodynamic psychotherapy is evidence-based; the effectiveness of psychoanalysis and its relationship to facts is disputed.
Intensive short-term dynamic psychotherapy (ISTDP) is a form of short-term psychotherapy developed through empirical, video-recorded research by Habib Davanloo.
Complex post-traumatic stress disorder (CPTSD) is a stress-related mental disorder generally occurring in response to complex traumas, i.e. commonly prolonged or repetitive exposures to a series of traumatic events, within which individuals perceive little or no chance to escape.
Dyadic developmental psychotherapy is a psychotherapeutic treatment method for families that have children with symptoms of emotional disorders, including complex trauma and disorders of attachment. It was originally developed by Arthur Becker-Weidman and Daniel Hughes as an intervention for children whose emotional distress resulted from earlier separation from familiar caregivers. Hughes cites attachment theory and particularly the work of John Bowlby as theoretical motivations for dyadic developmental psychotherapy.
Child psychotherapy, or mental health interventions for children refers to the psychological treatment of various mental disorders diagnosed in children and adolescents. The therapeutic techniques developed for younger age ranges specialize in prioritizing the relationship between the child and the therapist. The goal of maintaining positive therapist-client relationships is typically achieved using therapeutic conversations and can take place with the client alone, or through engagement with family members.
The conversational model of psychotherapy was devised by the English psychiatrist Robert Hobson, and developed by the Australian psychiatrist Russell Meares. Hobson listened to recordings of his own psychotherapeutic practice with more disturbed clients, and became aware of the ways in which a patient's self—their unique sense of personal being—can come alive and develop, or be destroyed, in the flux of the conversation in the consulting room.
Mentalization-based treatment (MBT) is an integrative form of psychotherapy, bringing together aspects of psychodynamic, cognitive-behavioral, systemic and ecological approaches. MBT was developed and manualised by Peter Fonagy and Anthony Bateman, designed for individuals with borderline personality disorder (BPD). Some of these individuals suffer from disorganized attachment and failed to develop a robust mentalization capacity. Fonagy and Bateman define mentalization as the process by which we implicitly and explicitly interpret the actions of oneself and others as meaningful on the basis of intentional mental states. The object of treatment is that patients with BPD increase their mentalization capacity, which should improve affect regulation, thereby reducing suicidality and self-harm, as well as strengthening interpersonal relationships.
Transference focused psychotherapy (TFP) is a highly structured, twice-weekly modified psychodynamic treatment based on Otto F. Kernberg's object relations model of borderline personality disorder. It views the individual with borderline personality organization (BPO) as holding unreconciled and contradictory internalized representations of self and significant others that are affectively charged. The defense against these contradictory internalized object relations leads to disturbed relationships with others and with self. The distorted perceptions of self, others, and associated affects are the focus of treatment as they emerge in the relationship with the therapist (transference). The treatment focuses on the integration of split off parts of self and object representations, and the consistent interpretation of these distorted perceptions is considered the mechanism of change.
The mainstay of management of borderline personality disorder is various forms of psychotherapy with medications being found to be of little use.
Schema therapy was developed by Jeffrey E. Young for use in treatment of personality disorders and chronic DSM Axis I disorders, such as when patients fail to respond or relapse after having been through other therapies. Schema therapy is an integrative psychotherapy combining theory and techniques from previously existing therapies, including cognitive behavioral therapy, psychoanalytic object relations theory, attachment theory, and Gestalt therapy.
Eclectic psychotherapy is a form of psychotherapy in which the clinician uses more than one theoretical approach, or multiple sets of techniques, to help with clients' needs. The use of different therapeutic approaches will be based on the effectiveness in resolving the patient's problems, rather than the theory behind each therapy.
In psychology, Trauma-informed feminist therapy is a model of trauma for both men and women that incorporates the client's sociopolitical context.
Imagery Rescripting is an experiential therapeutic technique that uses imagery and imagination to intervene in traumatic memories. The process is guided by a therapist who works with the client to define ways to work with particular traumatic memories, images, or nightmares.
References
- ↑ Gregory, R. J., Remen, A. L. (2008). A manual-based psychodynamic therapy for treatment-resistant borderline personality disorder. Psychotherapy: Theory, Research, Practice, Training, 45, 15-27.
- ↑ Gregory, R. J. (2007). Borderline attributions. American Journal of Psychotherapy, 61, 131-147.
- ↑ Gregory, R. J. (2005). The deconstructive experience. American Journal of Psychotherapy, 59, 295-305.
- ↑ Gregory, R. J. (2004). Thematic stages of recovery in the treatment of borderline personality disorder. American Journal of Psychotherapy, 58, 335-348.
- ↑ Schmahl, C., & Bremner, J. D. (2006). Neuroimaging in borderline personality disorder. Journal of Psychiatric Research, 40, 419-427.
- ↑ Lieberman, M. D., Eisenberger, N. I., Crockett, M. J., Tom, S. M., Pfeifer, J. H., & Way, B. M. (2007). Putting feelings into words: Affect labeling disrupts amygdala activity in response to affective stimuli. Psychological Science, 18, 421-428.
- ↑ Gregory, R. J., Chlebowski, S., Kang, D., Remen, A. L., Soderberg, M. G., Stepkovitch, J., Virk, S. (2008). A controlled trial of psychodynamic psychotherapy for co-occurring borderline personality disorder and alcohol use disorder. Psychotherapy: Theory, Research, Practice, Training, 45, 28-41.
- ↑ Gregory, R. J., Delucia-Deranja, E., & Mogle, J. A. (2010). Dynamic deconstructive psychotherapy versus optimized community care for borderline personality disorder co-occurring with alcohol use disorders: 30-month follow-up. Journal of Nervous and Mental Disease, 198, 292-298.
- ↑ Goldman, G. A., Gregory, R. J. (2009) Preliminary relationships between adherence and outcome in dynamic deconstructive psychotherapy. Psychotherapy: Theory, Research, Practice, Training, 46, 480-485.
- ↑ Goldman, G. A., & Gregory, R. J. (2010). Relationships between techniques and outcomes for borderline personality disorder. American Journal of Psychotherapy, 64, 359-371.
- ↑ Chlebowski, S., & Gregory, R. J. (2012). Three cases of dissociative identity disorder co-occurring with borderline personality disorder treated with dynamic deconstructive psychotherapy. American Journal of Psychotherapy, 66, 165-180.
- ↑ Sachdeva, S., Goldman, G., Mustata, G., Deranja, E., & Gregory, R. J. (2013). Naturalistic outcomes of evidence-based therapies for borderline personality disorder at a university clinic: A quasi-randomized trial. Journal of the American Psychoanalytic Association, 61, 578-584.