Radiation therapy or radiotherapy, often abbreviated RT, RTx, or XRT, is a therapy using ionizing radiation, generally provided as part of cancer treatment to control or kill malignant cells and normally delivered by a linear accelerator. Radiation therapy may be curative in a number of types of cancer if they are localized to one area of the body. It may also be used as part of adjuvant therapy, to prevent tumor recurrence after surgery to remove a primary malignant tumor. Radiation therapy is synergistic with chemotherapy, and has been used before, during, and after chemotherapy in susceptible cancers. The subspecialty of oncology concerned with radiotherapy is called radiation oncology. A physician who practices in this subspecialty is a radiation oncologist.

External beam radiotherapy (EBRT) is the most common form of radiotherapy. The patient sits or lies on a couch and an external source of ionizing radiation is pointed at a particular part of the body. In contrast to brachytherapy and unsealed source radiotherapy, in which the radiation source is inside the body, external beam radiotherapy directs the radiation at the tumour from outside the body. Orthovoltage ("superficial") X-rays are used for treating skin cancer and superficial structures. Megavoltage X-rays are used to treat deep-seated tumours, whereas megavoltage electron beams are typically used to treat superficial lesions extending to a depth of approximately 5 cm. X-rays and electron beams are by far the most widely used sources for external beam radiotherapy. A small number of centers operate experimental and pilot programs employing beams of heavier particles, particularly protons, owing to the rapid dropoff in absorbed dose beneath the depth of the target.

Orthovoltage X-rays are produced by X-ray tubes operating at voltages in the 100–500 kV range, and therefore the X-rays have a peak energy in the 100–500 keV range. Orthovoltage X-rays are sometimes termed "deep" X-rays (DXR). They cover the upper limit of energies used for diagnostic radiography, and are used in external beam radiotherapy to treat cancer and tumors. They penetrate tissue to a useful depth of about 4–6 cm. This makes them useful for treating skin, superficial tissues, and ribs, but not for deeper structures such as lungs or pelvic organs.

Brachytherapy is a form of radiation therapy where a sealed radiation source is placed inside or next to the area requiring treatment. Brachy is Greek for short. Brachytherapy is commonly used as an effective treatment for cervical, prostate, breast, esophageal and skin cancer and can also be used to treat tumours in many other body sites. Treatment results have demonstrated that the cancer-cure rates of brachytherapy are either comparable to surgery and external beam radiotherapy (EBRT) or are improved when used in combination with these techniques. Brachytherapy can be used alone or in combination with other therapies such as surgery, EBRT and chemotherapy.
Megavoltage X-rays are produced by linear accelerators ("linacs") operating at voltages in excess of 1000 kV (1 MV) range, and therefore have an energy in the MeV range. The voltage in this case refers to the voltage used to accelerate electrons in the linear accelerator and indicates the maximum possible energy of the photons which are subsequently produced. They are used in medicine in external beam radiotherapy to treat neoplasms, cancer and tumors. Beams with the voltage range of 4-25 MV are used to treat deeply buried cancers because radiation oncologists find that they penetrate well to deep sites within the body. Lower energy x-rays, called orthovoltage X-rays, are used to treat cancers closer to the surface.
The therapeutic index is a quantitative measurement of the relative safety of a drug. It is a comparison of the amount of a therapeutic agent that causes the therapeutic effect to the amount that causes toxicity. The related terms therapeutic window or safety window refer to a range of doses which optimize between efficacy and toxicity, achieving the greatest therapeutic benefit without resulting in unacceptable side-effects or toxicity.

In medicine, proton therapy, or proton radiotherapy, is a type of particle therapy that uses a beam of protons to irradiate diseased tissue, most often to treat cancer. The chief advantage of proton therapy over other types of external beam radiotherapy is that the dose of protons is deposited over a narrow range of depth; hence in minimal entry, exit, or scattered radiation dose to healthy nearby tissues.

Radiosurgery is surgery using radiation, that is, the destruction of precisely selected areas of tissue using ionizing radiation rather than excision with a blade. Like other forms of radiation therapy, it is usually used to treat cancer. Radiosurgery was originally defined by the Swedish neurosurgeon Lars Leksell as "a single high dose fraction of radiation, stereotactically directed to an intracranial region of interest".
A monitor unit (MU) is a measure of machine output from a clinical accelerator for radiation therapy such as a linear accelerator or an orthovoltage unit. Monitor units are measured by monitor chambers, which are ionization chambers that measure the dose delivered by a beam and are built into the treatment head of radiotherapy linear accelerators.

Fast neutron therapy utilizes high energy neutrons typically between 50 and 70 MeV to treat cancer. Most fast neutron therapy beams are produced by reactors, cyclotrons (d+Be) and linear accelerators. Neutron therapy is currently available in Germany, Russia, South Africa and the United States. In the United States, one treatment center is operational, in Seattle, Washington. The Seattle center uses a cyclotron which produces a proton beam impinging upon a beryllium target.

In radiotherapy, radiation treatment planning (RTP) is the process in which a team consisting of radiation oncologists, radiation therapist, medical physicists and medical dosimetrists plan the appropriate external beam radiotherapy or internal brachytherapy treatment technique for a patient with cancer.
Intraoperative radiation therapy (IORT) is radiation therapy that is administered during surgery directly in the operating room.

Cobalt therapy is the medical use of gamma rays from the radioisotope cobalt-60 to treat conditions such as cancer. Beginning in the 1950s, cobalt-60 was widely used in external beam radiotherapy (teletherapy) machines, which produced a beam of gamma rays which was directed into the patient's body to kill tumor tissue. Because these "cobalt machines" were expensive and required specialist support, they were often housed in cobalt units. Cobalt therapy was a revolutionary advance in radiotherapy in the post-World War II period but is now being replaced by other technologies such as linear accelerators.
Particle therapy is a form of external beam radiotherapy using beams of energetic neutrons, protons, or other heavier positive ions for cancer treatment. The most common type of particle therapy as of August 2021 is proton therapy.
Intraoperative electron radiation therapy is the application of electron radiation directly to the residual tumor or tumor bed during cancer surgery. Electron beams are useful for intraoperative radiation treatment because, depending on the electron energy, the dose falls off rapidly behind the target site, therefore sparing underlying healthy tissue.
Breast cancer management takes different approaches depending on physical and biological characteristics of the disease, as well as the age, over-all health and personal preferences of the patient. Treatment types can be classified into local therapy and systemic treatment. Local therapy is most efficacious in early stage breast cancer, while systemic therapy is generally justified in advanced and metastatic disease, or in diseases with specific phenotypes.

Targeted intra-operative radiotherapy, also known as targeted IORT, is a technique of giving radiotherapy to the tissues surrounding a cancer after its surgical removal, a form of intraoperative radiation therapy. The technique was designed in 1998 at the University College London. In patients having lumpectomy for breast cancer, the TARGIT-A(lone) randomized controlled trial tested whether TARGIT within a risk-adapted approach is non-inferior to conventional course of external beam postoperative radiotherapy given over several weeks.
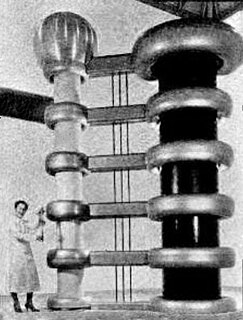
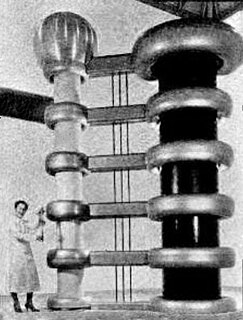
The history of radiation therapy or radiotherapy can be traced back to experiments made soon after the discovery of X-rays (1895), when it was shown that exposure to radiation produced cutaneous burns. Influenced by electrotherapy and escharotics — the medical application of caustic substances — doctors began using radiation to treat growths and lesions produced by diseases such as lupus, basal cell carcinoma, and epithelioma. Radiation was generally believed to have bactericidal properties, so when radium was discovered, in addition to treatments similar to those used with x-rays, it was also used as an additive to medical treatments for diseases such as tuberculosis where there were resistant bacilli.
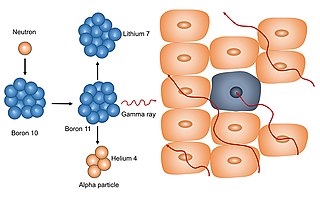
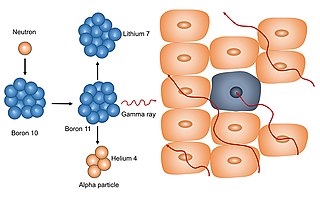
Neutron capture therapy (NCT) is a type of radiotherapy for treating locally invasive malignant tumors such as primary brain tumors, recurrent cancers of the head and neck region, and cutaneous and extracutaneous melanomas. It is a two-step process: first, the patient is injected with a tumor-localizing drug containing the stable isotope boron-10 (10B), which has a high propensity to capture low energy "thermal" neutrons. The neutron cross section of 10B is 1,000 times more than that of other elements, such as nitrogen, hydrogen, or oxygen, that occur in tissue. In the second step, the patient is radiated with epithermal neutrons, the sources of which in the past have been nuclear reactors and now are accelerators that produce higher energy epithermal neutrons. After losing energy as they penetrate tissue, the resultant low energy "thermal" neutrons are captured by the 10B atoms. The resulting decay reaction yields high-energy alpha particles that kill the cancer cells that have taken up enough 10B.
Auger therapy is a form of radiation therapy for the treatment of cancer which relies on low-energy electrons to damage cancer cells, rather than the high-energy radiation used in traditional radiation therapy. Similar to other forms of radiation therapy, Auger therapy relies on radiation-induced damage to cancer cells to arrest cell division, stop tumor growth and metastasis and kill cancerous cells. It differs from other types of radiation therapy in that electrons emitted via the Auger effect are released with low kinetic energy. In contrast to traditional α- and β-particle emitters, Auger electron emitters exhibit low cellular toxicity during transit in blood or bone marrow.