Related Research Articles

Organ donation is the process when a person authorizes an organ of their own to be removed and transplanted to another person, legally, either by consent while the donor is alive, through a legal authorization for deceased donation made prior to death, or for deceased donations through the authorization by the legal next of kin.

Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location. Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source.
Bioethics is both a field of study and professional practice, interested in ethical issues related to health, including those emerging from advances in biology, medicine, and technologies. It proposes the discussion about moral discernment in society and it is often related to medical policy and practice, but also to broader questions as environment, well-being and public health. Bioethics is concerned with the ethical questions that arise in the relationships among life sciences, biotechnology, medicine, politics, law, theology and philosophy. It includes the study of values relating to primary care, other branches of medicine, ethical education in science, animal, and environmental ethics, and public health.
Prior to the introduction of brain death into law in the mid to late 1970s, all organ transplants from cadaveric donors came from non-heart-beating donors (NHBDs).

Xenotransplantation, or heterologous transplant, is the transplantation of living cells, tissues or organs from one species to another. Such cells, tissues or organs are called xenografts or xenotransplants. It is contrasted with allotransplantation, syngeneic transplantation or isotransplantation and autotransplantation. Xenotransplantation is an artificial method of creating an animal-human chimera, that is, a human with a subset of animal cells. In contrast, an individual where each cell contains genetic material from a human and an animal is called a human–animal hybrid.
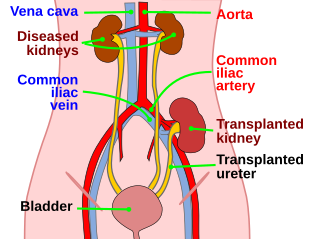
Kidney transplant or renal transplant is the organ transplant of a kidney into a patient with end-stage kidney disease (ESRD). Kidney transplant is typically classified as deceased-donor or living-donor transplantation depending on the source of the donor organ. Living-donor kidney transplants are further characterized as genetically related (living-related) or non-related (living-unrelated) transplants, depending on whether a biological relationship exists between the donor and recipient. The first successful kidney transplant was performed in 1954 by a team including Joseph Murray, the recipient’s surgeon, and Hartwell Harrison, surgeon for the donor. Murray was awarded a Nobel Prize in Physiology or Medicine in 1990 for this and other work. In 2018, an estimated 95,479 kidney transplants were performed worldwide, 36% of which came from living donors.

Organ transplantation in China has taken place since the 1960s, and is one of the largest organ transplant programmes in the world, peaking at over 13,000 liver and kidney transplants a year in 2004.
Organ procurement is a surgical procedure that removes organs or tissues for reuse, typically for organ transplantation.
Nancy Scheper-Hughes is an anthropologist, educator and author. She is the Chancellor's Professor Emerita of Anthropology and the director and co-founder of the PhD program in Critical Medical Anthropology at the University of California, Berkeley. She is known for her writing on the anthropology of the body, hunger, illness, medicine, motherhood, psychiatry, psychosis, social suffering, violence and genocide, death squads, and human trafficking.
Certain fundamental Jewish law questions arise in issues of organ donation. Donation of an organ from a living person to save another's life, where the donor's health will not appreciably suffer, is permitted and encouraged in Jewish law. Donation of an organ from a dead person is equally permitted for the same purpose: to save a life. This simple statement of the issue belies, however, the complexity of defining death in Jewish law. Thus, although there are side issues regarding mutilation of the body etc., the primary issue that prevents organ donation from the dead amongst Jews, in many cases, is the definition of death, simply because to take a life-sustaining organ from a person who was still alive would be murder.

The National Organ Transplant Act (NOTA) of 1984 is an Act of the United States Congress that created the framework for the organ transplant system in the country. The act provided clarity on the property rights of human organs obtained from deceased individuals and established a public-private partnership known as Organ Procurement and Transplantation Network (OPTN). The OPTN was given the authority to oversee the national distribution of organs.

Sigrid Fry-Revere is an American medical ethicist and lawyer who has worked on many issues in patient care ethics, but most recently has been working on the rights of living organ donors.
Organ trade is the trading of human organs, tissues, or other body products, usually for transplantation. According to the World Health Organization (WHO), organ trade is a commercial transplantation where there is a profit, or transplantations that occur outside of national medical systems. There is a global need or demand for healthy body parts for transplantation, which exceeds the numbers available.

The Kilgour–Matas report is a 2006/2007 investigative report into allegations of live organ harvesting in China conducted by Canadian MP David Kilgour and human rights lawyer David Matas. The report was requested by the Coalition to Investigate the Persecution of Falun Gong (CIPFG) after allegations emerged that Falun Gong practitioners were secretly having their organs removed against their will at Sujiatun Thrombosis Hospital. The report, based on circumstantial evidence, concluded that "there has been, and continues today to be, large-scale organ seizures from unwilling Falun Gong practitioners." China has consistently denied the allegations.
Organ transplantation in Israel has historically been low compared to other Western countries due to a common belief that organ donation is prohibited under Jewish law. This changed with the passage of new organ donation laws in 2008. If two patients have the same medical need, priority will now go to the patient who has signed an organ donor card, or whose family members have donated an organ. This policy was nicknamed don't give, don't get. The law also defines "brain death" as an indication of death for all legal purposes, including organ donation. Additionally the law provides financial reimbursement to living donors for medical expenses due to donation and lost time at work. Organ trafficking is explicitly banned. Health insurance plans can no longer reimburse patients who go abroad to receive transplants.
Many different major religious groups and denominations have varying views on organ donation of a deceased and live bodies, depending on their ideologies. Differing opinions can arise depending on if the death is categorized as brain death or cease of the heartbeat. It is important for doctors and health care providers to be knowledgeable about differentiating theological and cultural views on death and organ donations as nations are becoming more multicultural.
The Declaration of Istanbul was created at the Istanbul Summit on Organ Trafficking and Transplant Tourism held from 30 April to 1 May 2008 in Istanbul, Turkey. The Declaration clarifies the issues of transplant tourism, trafficking and commercialism and provides ethical guidelines for practice in organ donation and transplantation. Since the creation of the declaration, over 100 countries have endorsed the principles. Some nations have subsequently strengthened their laws against commercial organ trade, including China, Israel, the Philippines, and Pakistan.
Organ donation in the United States prison population is the donation of biological tissues or organs from incarcerated individuals to living recipients in need of a transplantation.
Allegations of forced organ harvesting from Falun Gong practitioners and other political prisoners in China have raised concern within the international community. According to a report by former lawmaker David Kilgour, human rights lawyer David Matas and journalist Ethan Gutmann of the Victims of Communism Memorial Foundation, political prisoners, mainly Falun Gong practitioners, are being executed "on demand" in order to provide organs for transplant to recipients. Reports have said that organ harvesting has been used to advance the Chinese Communist Party's persecution of Falun Gong and because of the financial incentives available to the institutions and individuals involved in the trade. A report by The Washington Post has disputed some of the allegations, saying that China does not import sufficient quantities of immunosuppressant drugs, used by transplant recipients, to carry out such quantities of organ harvesting.
Organ donation is when a person gives their organs after they die to someone in need of new organs. Transplantation is the process of transplanting the organs donated into another person. This process extends the life expectancy of a person suffering from organ failure. The number of patients requiring organ transplants outweighs the number of donor organs available.
References
- ↑ Bulletin of the World Health Organization, World Health Organization, Volume 85, Number 1, January 2007, 1-84
- ↑ Organ trafficking and transplantation pose new challenges, Bulletin of the World Health Organization, Volume 82, Number 9, September 2004, 639-718
- ↑ Hillman H. Harvesting organs from recently executed prisoners: Practice must be stopped. British Medical Journal, 2001; 323(7323):1254.
- ↑ New era for organ donation and transplant in China, by World Health Organization, Volume 90, Number 11, November 2012, 793-868
- ↑ Whetstine L, Streat S, Darwin M, Crippen D (2005). "Pro/con ethics debate: When is dead really dead?". Critical Care. 9 (6): 538–42. doi: 10.1186/cc3894 . PMC 1414041 . PMID 16356234.
- ↑ Keeping kidneys, Bulletin of the World Health Organization, Volume 90, Number 10, October 2012, 713-792
- ↑ Drawing the ethical line between organ transplantation and lifestyle abuse. E H Kluge, CMAJ. 1994 March 1; 150(5): 745–746.
- ↑ Take My Kidney, Please
- ↑ Bulletin of the World Health Organization 2010;88:870-872. doi: 10.2471/BLT.09.074542
- ↑ Levenson, James L.; Olbrisch, Mary Ellen (1993). "Psychosocial Evaluation of Organ Transplant Candidates". Psychosomatics. 34 (4): 314–323. doi:10.1016/S0033-3182(93)71865-4. PMID 8351306.
- ↑ Ross, Lainie Friedman (2021). "Ethics of Organ Transplantation in Persons with Intellectual Disability". The Journal of Pediatrics. 235: 6–9. doi:10.1016/j.jpeds.2021.05.046. ISSN 0022-3476. PMID 34029600. S2CID 243315184.
- ↑ Statter, Mindy B.; Noritz, Garey (2020-04-20). "Children With Intellectual and Developmental Disabilities as Organ Transplantation Recipients". Pediatrics. 145 (5): e20200625. doi: 10.1542/peds.2020-0625 . ISSN 0031-4005. PMID 32312907.