Ultrasound is sound with frequencies greater than 20 kilohertz. This frequency is the approximate upper audible limit of human hearing in healthy young adults. The physical principles of acoustic waves apply to any frequency range, including ultrasound. Ultrasonic devices operate with frequencies from 20 kHz up to several gigahertz.

Medical ultrasound includes diagnostic techniques using ultrasound, as well as therapeutic applications of ultrasound. In diagnosis, it is used to create an image of internal body structures such as tendons, muscles, joints, blood vessels, and internal organs, to measure some characteristics or to generate an informative audible sound. The usage of ultrasound to produce visual images for medicine is called medical ultrasonography or simply sonography, or echography. The practice of examining pregnant women using ultrasound is called obstetric ultrasonography, and was an early development of clinical ultrasonography. The machine used is called an ultrasound machine, a sonograph or an echograph. The visual image formed using this technique is called an ultrasonogram, a sonogram or an echogram.
Sonophoresis also known as phonophoresis, is a method that utilizes ultrasound to enhance the delivery of topical medications through the stratum corneum, to the epidermis and dermis. Sonophoresis allows for the enhancement of the permeability of the skin along with other modalities, such as iontophoresis, to deliver drugs with lesser side effects. Currently, sonophoresis is used widely in transdermal drug delivery, but has potential applications in other sectors of drug delivery, such as the delivery of drugs to the eye and brain.

3D ultrasound is a medical ultrasound technique, often used in fetal, cardiac, trans-rectal and intra-vascular applications. 3D ultrasound refers specifically to the volume rendering of ultrasound data. When involving a series of 3D volumes collected over time, it can also be referred to as 4D ultrasound or real-time 3D ultrasound.
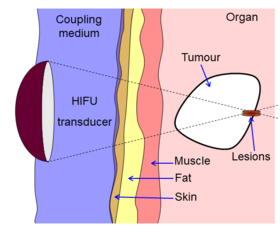
Therapeutic ultrasound refers generally to any type of ultrasonic procedure that uses ultrasound for therapeutic benefit. Physiotherapeutic ultrasound was introduced into clinical practice in the 1950s, with lithotripsy introduced in the 1980s. Others are at various stages in transitioning from research to clinical use: HIFU, targeted ultrasound drug delivery, trans-dermal ultrasound drug delivery, ultrasound hemostasis, cancer therapy, and ultrasound assisted thrombolysis It may use focused ultrasound or unfocused ultrasound.
Ultrasound energy, simply known as ultrasound, is a type of mechanical energy called sound characterized by vibrating or moving particles within a medium. Ultrasound is distinguished by vibrations with a frequency greater than 20,000 Hz, compared to audible sounds that humans typically hear with frequencies between 20 and 20,000 Hz. Ultrasound energy requires matter or a medium with particles to vibrate to conduct or propagate its energy. The energy generally travels through most mediums in the form of a wave in which particles are deformed or displaced by the energy then reestablished after the energy passes. Types of waves include shear, surface, and longitudinal waves with the latter being one of the most common used in biological applications. The characteristics of the traveling ultrasound energy greatly depend on the medium that it is traveling through. While ultrasound waves propagate through a medium, the amplitude of the wave is continually reduced or weakened with the distance it travels. This is known as attenuation and is due to the scattering or deflecting of energy signals as the wave propagates and the conversion of some of the energy to heat energy within the medium. A medium that changes the mechanical energy from the vibrations of the ultrasound energy into thermal or heat energy is called viscoelastic. The properties of ultrasound waves traveling through the medium of biological tissues has been extensively studied in recent years and implemented into many important medical tools.
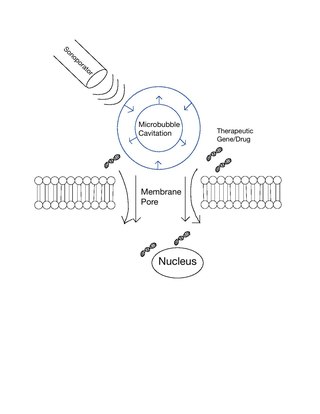
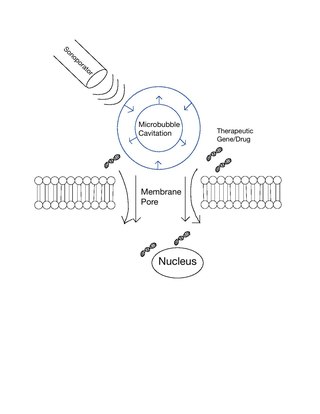
Sonoporation, or cellular sonication, is the use of sound in the ultrasonic range for increasing the permeability of the cell plasma membrane. This technique is usually used in molecular biology and non-viral gene therapy in order to allow uptake of large molecules such as DNA into the cell, in a cell disruption process called transfection or transformation. Sonoporation employs the acoustic cavitation of microbubbles to enhance delivery of these large molecules. The exact mechanism of sonoporation-mediated membrane translocation remains unclear, with a few different hypotheses currently being explored.
Treatment for prostate cancer may involve active surveillance, surgery, radiation therapy – including brachytherapy and external-beam radiation therapy, proton therapy, high-intensity focused ultrasound (HIFU), cryosurgery, hormonal therapy, chemotherapy, or some combination. Treatments also extend to survivorship based interventions. These interventions are focused on five domains including: physical symptoms, psychological symptoms, surveillance, health promotion and care coordination. However, a published review has found only high levels of evidence for interventions that target physical and psychological symptom management and health promotion, with no reviews of interventions for either care coordination or surveillance. The favored treatment option depends on the stage of the disease, the Gleason score, and the PSA level. Other important factors include the man's age, his general health, and his feelings about potential treatments and their possible side-effects. Because all treatments can have significant side-effects, such as erectile dysfunction and urinary incontinence, treatment discussions often focus on balancing the goals of therapy with the risks of lifestyle alterations.
Microbubbles are bubbles smaller than one hundredth of a millimetre in diameter, but larger than one micrometre. They have widespread application in industry, medicine, life science, and food technology. The composition of the bubble shell and filling material determine important design features such as buoyancy, crush strength, thermal conductivity, and acoustic properties.

Sonalleve MR-HIFU is a medical system developed by Philips Healthcare for the treatment of uterine fibroids without surgery. The system uses non-invasive high-intensity focused ultrasound (HIFU) guided by magnetic resonance (MR), whence the acronym MR-HIFU. The procedure involves volumetric heating of fibroids with real-time feedback. In June 2017, Philips and Profound Medical announced an agreement to transfer Philips' MR-HIFU business, which includes the Sonalleve system, to Profound Medical.

Sonodynamic therapy (SDT) is a noninvasive treatment, often used for tumor irradiation, that utilizes a sonosensitizer and the deep penetration of ultrasound to treat lesions of varying depths by reducing target cell number and preventing future tumor growth. Many existing cancer treatment strategies cause systemic toxicity or cannot penetrate tissue deep enough to reach the entire tumor; however, emerging ultrasound stimulated therapies could offer an alternative to these treatments with their increased efficiency, greater penetration depth, and reduced side effects. Sonodynamic therapy could be used to treat cancers and other diseases, such as atherosclerosis, and diminish the risk associated with other treatment strategies since it induces cytotoxic effects only when externally stimulated by ultrasound and only at the cancerous region, as opposed to the systemic administration of chemotherapy drugs.
Nadine Barrie Smith (1962–2010) was an American biomedical researcher in the field of therapeutic ultrasound and non-invasive drug delivery. She was also an educator and mentor, especially to women students.
Interventional oncology is a subspecialty field of interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments to allow targeted and precise treatment of solid tumours located in various organs of the human body, including but not limited to the liver, kidneys, lungs, and bones. Interventional oncology treatments are routinely carried out by interventional radiologists in appropriate settings and facilities.
This is a historical timeline of the development and progress of cancer treatments, which includes time of discovery, progress, and approval of the treatments.
Combinatorial ablation and immunotherapy is an oncological treatment that combines various tumor-ablation techniques with immunotherapy treatment. Combining ablation therapy of tumors with immunotherapy enhances the immunostimulating response and has synergistic effects for curative metastatic cancer treatment. Various ablative techniques are utilized including cryoablation, radiofrequency ablation, laser ablation, photodynamic ablation, stereotactic radiation therapy, alpha-emitting radiation therapy, hyperthermia therapy, HIFU. Thus, combinatorial ablation of tumors and immunotherapy is a way of achieving an autologous, in-vivo tumor lysate vaccine and treating metastatic disease.
Hashim U. Ahmed is a British surgeon, medical researcher and author of publications in the field of prostate cancer diagnostics and treatment; his research has contributed to changes in the way men with suspected prostate cancer and men with prostate enlargement are diagnosed and treated. He is Professor and Chair of Urology at Imperial College Healthcare NHS Trust and Consultant Urological Surgeon at both Charing Cross Hospital and BUPA Cromwell Hospital.

Katherine Whittaker Ferrara is an American engineer who is a professor of radiology at Stanford University. Ferrara has been elected a Fellow of the American Association for the Advancement of Science, Institute of Electrical and Electronics Engineers and American Institute for Medical and Biological Engineering.

Focused ultrasound for intracrainial drug delivery is a non-invasive technique that uses high-frequency sound waves to disrupt tight junctions in the blood–brain barrier (BBB), allowing for increased passage of therapeutics into the brain. The BBB normally blocks nearly 98% of drugs from accessing the central nervous system, so FUS has the potential to address a major challenge in intracranial drug delivery by providing targeted and reversible BBB disruption. Using FUS to enhance drug delivery to the brain could significantly improve patient outcomes for a variety of diseases including Alzheimer's disease, Parkinson's disease, and brain cancer.
Ultrasound-triggered drug delivery using stimuli-responsive hydrogels refers to the process of using ultrasound energy for inducing drug release from hydrogels that are sensitive to acoustic stimuli. This method of approach is one of many stimuli-responsive drug delivery-based systems that has gained traction in recent years due to its demonstration of localization and specificity of disease treatment. Although recent developments in this field highlight its potential in treating certain diseases such as COVID-19, there remain many major challenges that need to be addressed and overcome before more related biomedical applications are clinically translated into standard of care.
Focused-ultrasound-mediated diagnostics or FUS-mediated diagnostics are an area of clinical diagnostic tools that use ultrasound to detect diseases and cancers. Although ultrasound has been used for imaging in various settings, focused-ultrasound refers to the detection of specific cells and biomarkers under flow combining ultrasound with lasers, microbubbles, and imaging techniques. Current diagnostic techniques for detecting tumors and diseases using biopsies often include invasive procedures and require improved accuracy, especially in cases such as glioblastoma and melanoma. The field of FUS-mediated diagnostics targeting cells and biomarkers is being investigated for overcoming these limitations.