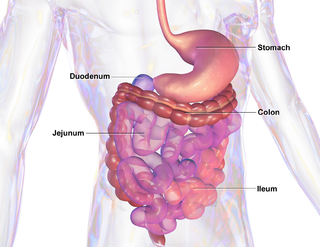
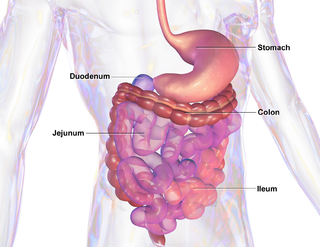
In anatomy, a polyp is an abnormal growth of tissue projecting from a mucous membrane. If it is attached to the surface by a narrow elongated stalk, it is said to be pedunculated; if it is attached without a stalk, it is said to be sessile. Polyps are commonly found in the colon, stomach, nose, ear, sinus(es), urinary bladder, and uterus. They may also occur elsewhere in the body where there are mucous membranes, including the cervix, vocal folds, and small intestine. Some polyps are tumors (neoplasms) and others are non-neoplastic, for example hyperplastic or dysplastic, which are benign. The neoplastic ones are usually benign, although some can be pre-malignant, or concurrent with a malignancy.

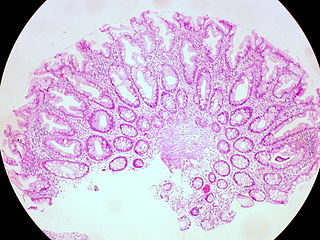
An adenoma is a benign tumor of epithelial tissue with glandular origin, glandular characteristics, or both. Adenomas can grow from many glandular organs, including the adrenal glands, pituitary gland, thyroid, prostate, and others. Some adenomas grow from epithelial tissue in nonglandular areas but express glandular tissue structure. Although adenomas are benign, they should be treated as pre-cancerous. Over time adenomas may transform to become malignant, at which point they are called adenocarcinomas. Most adenomas do not transform. However, even though benign, they have the potential to cause serious health complications by compressing other structures and by producing large amounts of hormones in an unregulated, non-feedback-dependent manner. Some adenomas are too small to be seen macroscopically but can still cause clinical symptoms.

Gardner's syndrome is a subtype of familial adenomatous polyposis (FAP). Gardner syndrome is an autosomal dominant form of polyposis characterized by the presence of multiple polyps in the colon together with tumors outside the colon. The extracolonic tumors may include osteomas of the skull, thyroid cancer, epidermoid cysts, fibromas, as well as the occurrence of desmoid tumors in approximately 15% of affected individuals.

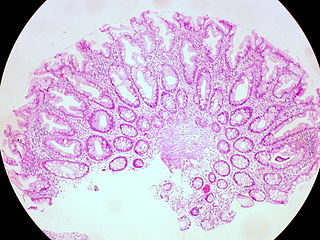
Familial adenomatous polyposis (FAP) is an autosomal dominant inherited condition in which numerous adenomatous polyps form mainly in the epithelium of the large intestine. While these polyps start out benign, malignant transformation into colon cancer occurs when they are left untreated. Three variants are known to exist, FAP and attenuated FAP are caused by APC gene defects on chromosome 5 while autosomal recessive FAP is caused by defects in the MUTYH gene on chromosome 1. Of the three, FAP itself is the most severe and most common; although for all three, the resulting colonic polyps and cancers are initially confined to the colon wall. Detection and removal before metastasis outside the colon can greatly reduce and in many cases eliminate the spread of cancer.

A benign tumor is a mass of cells (tumor) that does not invade neighboring tissue or metastasize. Compared to malignant (cancerous) tumors, benign tumors generally have a slower growth rate. Benign tumors have relatively well differentiated cells. They are often surrounded by an outer surface or stay contained within the epithelium. Common examples of benign tumors include moles and uterine fibroids.

Hepatoblastoma is a malignant liver cancer occurring in infants and children and composed of tissue resembling fetal liver cells, mature liver cells, or bile duct cells. They usually present with an abdominal mass. The disease is most commonly diagnosed during a child's first three years of life. Alpha-fetoprotein (AFP) levels are commonly elevated, but when AFP is not elevated at diagnosis the prognosis is poor.
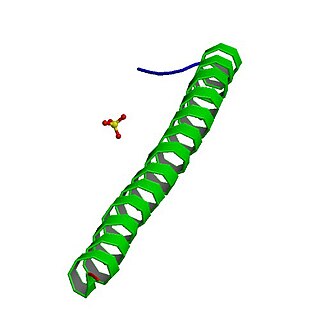
Adenomatous polyposis coli (APC) also known as deleted in polyposis 2.5 (DP2.5) is a protein that in humans is encoded by the APC gene. The APC protein is a negative regulator that controls beta-catenin concentrations and interacts with E-cadherin, which are involved in cell adhesion. Mutations in the APC gene may result in colorectal cancer and desmoid tumors.

MUTYH is a human gene that encodes a DNA glycosylase, MUTYH glycosylase. It is involved in oxidative DNA damage repair and is part of the base excision repair pathway. The enzyme excises adenine bases from the DNA backbone at sites where adenine is inappropriately paired with guanine, cytosine, or 8-oxo-7,8-dihydroguanine, a common form of oxidative DNA damage.

Aggressive fibromatosis or desmoid tumor is a rare condition. Desmoid tumors are a type of fibromatosis and related to sarcoma, though without the ability to spread throughout the body (metastasize). The tumors arise from cells called fibroblasts, which are found throughout the body and provide structural support, protection to the vital organs, and play a critical role in wound healing. These tumors tend to occur in women in their thirties, but can occur in anyone at any age. They can be either relatively slow-growing or malignant. However, aggressive fibromatosis is locally aggressive and can cause life-threatening problems or even death when the tumors compress vital organs such as intestines, kidneys, lungs, blood vessels, or nerves. The condition is rarely fatal. Most cases are sporadic, but some are associated with familial adenomatous polyposis (FAP). Approximately 10% of individuals with Gardner's syndrome, a type of FAP with extracolonic features, have desmoid tumors.
Cronkhite–Canada syndrome is a rare syndrome characterized by multiple polyps of the digestive tract. It is sporadic, and it is currently considered acquired and idiopathic.

Juvenile polyposis syndrome is an autosomal dominant genetic condition characterized by the appearance of multiple juvenile polyps in the gastrointestinal tract. Polyps are abnormal growths arising from a mucous membrane. These usually begin appearing before age 20, but the term juvenile refers to the type of polyp, not to the age of the affected person. While the majority of the polyps found in juvenile polyposis syndrome are non-neoplastic, hamartomatous, self-limiting and benign, there is an increased risk of adenocarcinoma.

A colorectal polyp is a polyp occurring on the lining of the colon or rectum. Untreated colorectal polyps can develop into colorectal cancer.

A sessile serrated lesion (SSL) is a premalignant flat lesion of the colon, predominantly seen in the cecum and ascending colon.
APC, WNT signaling pathway regulator is a protein that in humans is encoded by the APC gene.
MUTYH-associated polyposis is an autosomal recessive polyposis syndrome. The disorder is caused by mutations in both alleles of the DNA repair gene, MUTYH. The MUTYH gene encodes a base excision repair protein, which corrects oxidative damage to DNA. Affected individuals have an increased risk of colorectal cancer, precancerous colon polyps (adenomas) and an increased risk of several additional cancers. About 1–2 percent of the population possess a mutated copy of the MUTYH gene, and less than 1 percent of people have the MUTYH associated polyposis syndrome. The presence of 10 or more colon adenomas should prompt consideration of MUTYH-associated polyposis, familial adenomatous polyposis and similar syndromes.
Serrated polyposis syndrome (SPS), previously known as hyperplastic polyposis syndrome, is a disorder characterized by the appearance of serrated polyps in the colon. While serrated polyposis syndrome does not cause symptoms, the condition is associated with a higher risk of colorectal cancer (CRC). The lifelong risk of CRC is between 25 and 40%. SPS is the most common polyposis syndrome affecting the colon, but is under recognized due to a lack of systemic long term monitoring. Diagnosis requires colonoscopy, and is defined by the presence of either of two criteria: ≥5 serrated lesions/polyps proximal to the rectum, or >20 serrated lesions/polyps of any size distributed throughout the colon with 5 proximal to the rectum.
Polymerase proofreading-associated polyposis (PPAP) is an autosomal dominant hereditary cancer syndrome, which is characterized by numerous polyps in the colon and an increased risk of colorectal cancer. It is caused by germline mutations in DNA polymerase ε (POLE) and δ (POLD1). Affected individuals develop numerous polyps called colorectal adenomas. Compared with other polyposis syndromes, Polymerase proofreading-associated polyposis is rare. Genetic testing can help exclude similar syndromes, such as Familial adenomatous polyposis and MUTYH-associated polyposis. Endometrial cancer, duodenal polyps and duodenal cancer may also occur.
Juvenile polyps are a type of polyp found in the colon. While juvenile polyps are typically found in children, they may be found in people of any age. Juvenile polyps are a type of hamartomatous polyps, which consist of a disorganized mass of tissue. They occur in about two percent of children. Juvenile polyps often do not cause symptoms (asymptomatic); when present, symptoms usually include gastrointestinal bleeding and prolapse through the rectum. Removal of the polyp (polypectomy) is warranted when symptoms are present, for treatment and definite histopathological diagnosis. In the absence of symptoms, removal is not necessary. Recurrence of polyps following removal is relatively common. Juvenile polyps are usually sporadic, occurring in isolation, although they may occur as a part of juvenile polyposis syndrome. Sporadic juvenile polyps may occur in any part of the colon, but are usually found in the distal colon. In contrast to other types of colon polyps, juvenile polyps are not premalignant and are not usually associated with a higher risk of cancer; however, individuals with juvenile polyposis syndrome are at increased risk of gastric and colorectal cancer., Unlike juvenile polyposis syndrome, solitary juvenile polyps do not require follow up with surveillance colonoscopy.

A fundic gland polyp is a type of polyp, found in the fundus of the stomach. Fundic gland polyps are found in 0.8 to 1.9% of patients who undergo esophagogastroduodenoscopy, and are more common in middle-aged women.
Gardner fibroma (GF) is a benign fibroblastic tumor. GF tumors typically develop in the dermis and adjacent subcutaneous tissue lying just below the dermis. These tumors typically occur on the back, abdomen, and other superficial sites but in rare cases have been diagnoses in internal sites such as the retroperitoneum and around the large blood vessels in the upper thoracic cavity. The World Health Organization, 2020, classified Gardner fibroma as a benign tumor in the category of fibroblastic and myofibroblastic tumors.