Health care reform is for the most part governmental policy that affects health care delivery in a given place. Health care reform typically attempts to:
A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.
Health insurance or medical insurance is a type of insurance that covers the whole or a part of the risk of a person incurring medical expenses. As with other types of insurance, risk is shared among many individuals. By estimating the overall risk of health risk and health system expenses over the risk pool, an insurer can develop a routine finance structure, such as a monthly premium or payroll tax, to provide the money to pay for the health care benefits specified in the insurance agreement. The benefit is administered by a central organization, such as a government agency, private business, or not-for-profit entity.
Universal health care is a health care system in which all residents of a particular country or region are assured access to health care. It is generally organized around providing either all residents or only those who cannot afford on their own, with either health services or the means to acquire them, with the end goal of improving health outcomes.
Health care in Ireland is delivered through public and private healthcare. The public health care system is governed by the Health Act 2004, which established a new body to be responsible for providing health and personal social services to everyone living in Ireland – the Health Service Executive. The new national health service came into being officially on 1 January 2005; however the new structures are currently in the process of being established as the reform programme continues. In addition to the public-sector, there is also a large private healthcare market.
The healthcare in Switzerland is universal and is regulated by the Swiss Federal Law on Health Insurance. There are no free state-provided health services, but private health insurance is compulsory for all persons residing in Switzerland.

Germany has a universal multi-payer health care system paid for by a combination of statutory health insurance and private health insurance.

Healthcare in Russia is provided by the state through the Federal Compulsory Medical Insurance Fund, and regulated through the Ministry of Health. The Constitution of the Russian Federation has provided all citizens the right to free healthcare since 1993. In 2008, 621,000 doctors and 1.3 million nurses were employed in Russian healthcare. The number of doctors per 10,000 people was 43.8, but only 12.1 in rural areas. The number of general practitioners as a share of the total number of doctors was 1.26 percent. There are about 9.3 beds per thousand population—nearly double the OECD average.

Healthcare in Turkey consists of a mix of public and private health services. Turkey introduced universal health care in 2003. Known as Universal Health Insurance Genel Sağlık Sigortası, it is funded by a tax surcharge on employers, currently at 5%. Public-sector funding covers approximately 75.2% of health expenditures.
Healthcare in Finland consists of a highly decentralized three-level publicly funded healthcare system and a much smaller private sector. Although the Ministry of Social Affairs and Health has the highest decision-making authority, the municipalities are responsible for providing healthcare to their residents.
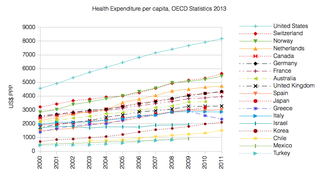
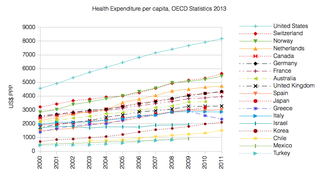
The French health care system is one of universal health care largely financed by government national health insurance. In its 2000 assessment of world health care systems, the World Health Organization found that France provided the "best overall health care" in the world. In 2017, France spent 11.3% of GDP on health care, or US$5,370 per capita, a figure higher than the average spent by rich countries, though similar to Germany (10.6%) and Canada (10%), but much less than in the US. Approximately 77% of health expenditures are covered by government funded agencies.

Spain operates a universal health care system. According to the Organisation for Economic Co-operation and Development, total health spending accounted for 9.4% of GDP in Spain in 2011, slightly above the OECD average of 9.3%. The Spanish health care system is ranked as the 7th most efficient healthcare in the world, as indicated in the year 2000 in a report by the World Health Organization. Spain's healthcare system ranks 19th in Europe according to the 2018 Euro health consumer index. Spain is ranked 1st in the world in organ transplants.
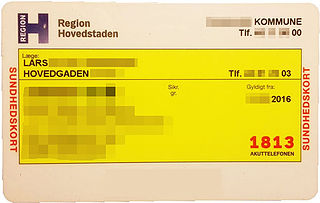
Healthcare in Denmark is largely provided by the local governments of the five regions, with coordination and regulation by central government, while nursing homes, home care, and school health services are the responsibility of the 98 municipalities. Some specialised hospital services are managed centrally.

Hungary has a tax-funded universal healthcare system, organized by the state-owned National Health Insurance Fund. While healthcare is considered universal, several reasons persist preventing Hungarian nationals to access healthcare services. For instance, a Hungarian citizen who lived abroad but is unable to show contributions to another country's healthcare system will not be able to access the Hungarian healthcare system free of charge. However, to the OECD, 100% of the total population is covered by universal health insurance, which is absolutely free for children, mothers or fathers with babies, students, pensioners, people with low income, handicapped people, priests and other church employees. In 2022 the cost of public health insurance is 8,400 HUF per month which is the equivalent of $23.69. The healthcare system underwent significant changes which also resulted in improving life expectancy and a very low infant mortality rate. According to the OECD Hungary spent 7.8% of its GDP on health care in 2012. Total health expenditure was $US1,688.7 per capita in 2011, US$1,098.3governmental-fund (65%) and US$590.4 private-fund (35%).

Healthcare in Slovenia is organised primarily through the Health Insurance Institute of Slovenia. In 2015, healthcare expenditures accounted for 8.10% of GDP. The Slovenian healthcare system was ranked 15th in the Euro health consumer index 2015. The country ranked second in the 2012 Euro Hepatitis Index.
This article provides a brief overview of the health care systems of the world, sorted by continent.

A new measure of expected human capital calculated for 195 countries from 1990 to 2016 and defined for each birth cohort as the expected years lived from age 20 to 64 years and adjusted for educational attainment, learning or education quality, and functional health status was published by The Lancet in September 2018. Latvia had the twenty-first highest level of expected human capital with 23 health, education, and learning-adjusted expected years lived between age 20 and 64 years.

As of 2019 Lithuanian life expectancy at birth was 76.0 and the infant mortality rate was 2.99 per 1,000 births. This is below the EU and OECD average.

The Czech Republic has a universal health care system, based on a compulsory insurance model, with fee-for-service care funded by mandatory employment-related insurance plans since 1992. According to the 2018 Euro health consumer index, a comparison of healthcare in Europe, the Czech healthcare is ranked 14th, just behind Portugal and two positions ahead of the United Kingdom.