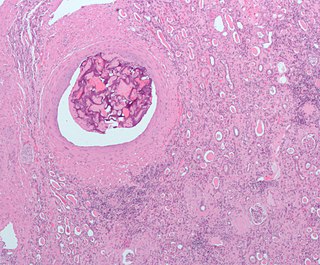
An embolism is the lodging of an embolus, a blockage-causing piece of material, inside a blood vessel. The embolus may be a blood clot (thrombus), a fat globule, a bubble of air or other gas, amniotic fluid, or foreign material.
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction.
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.
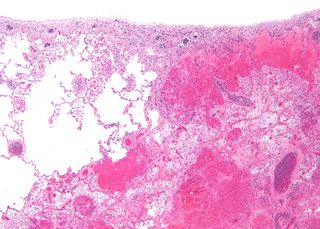
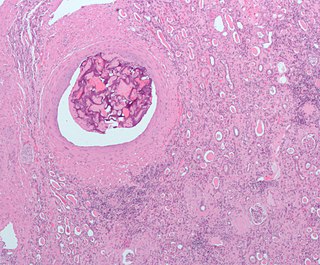
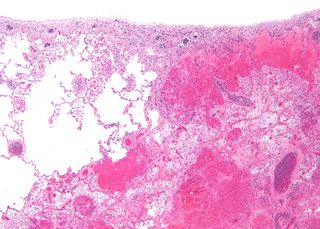
Infarction is tissue death (necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct (from the Latin infarctus, "stuffed into").

Stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functioning properly.

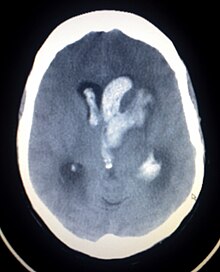
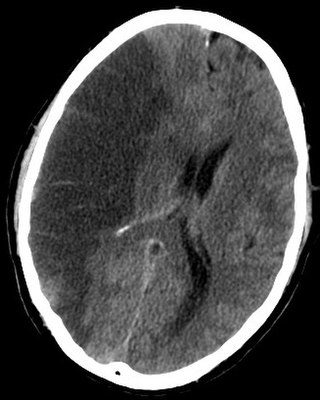
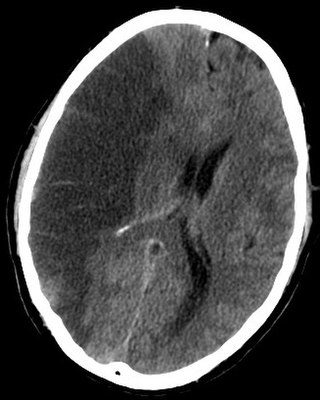
Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consciousness, fever, weakness, numbness, and sometimes seizures. Neck stiffness or neck pain are also relatively common. In about a quarter of people a small bleed with resolving symptoms occurs within a month of a larger bleed.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.

Cerebral hypoxia is a form of hypoxia, specifically involving the brain; when the brain is completely deprived of oxygen, it is called cerebral anoxia. There are four categories of cerebral hypoxia; they are, in order of increasing severity: diffuse cerebral hypoxia (DCH), focal cerebral ischemia, cerebral infarction, and global cerebral ischemia. Prolonged hypoxia induces neuronal cell death via apoptosis, resulting in a hypoxic brain injury.

Intraparenchymal hemorrhage (IPH) is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage (IVH).

Cerebral infarction, also known as an ischemic stroke, is the pathologic process that results in an area of necrotic tissue in the brain. In mid to high income countries, a stroke is the main reason for disability among people and the 2nd cause of death. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia). This is most commonly due to a thrombotic occlusion, or an embolic occlusion of major vessels which leads to a cerebral infarct. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.
An embolus, is described as a free-floating mass, located inside blood vessels that can travel from one site in the blood stream to another. An embolus can be made up of solid, liquid, or gas. Once these masses get "stuck" in a different blood vessel, it is then known as an "embolism." An embolism can cause ischemia—damage to an organ from lack of oxygen. A paradoxical embolism is a specific type of embolism in which the embolus travels from the right side of the heart to the left side of the heart and lodges itself in a blood vessel known as an artery. Thus, it is termed "paradoxical" because the embolus lands in an artery, rather than a vein.

A watershed stroke is defined as a brain ischemia that is localized to the vulnerable border zones between the tissues supplied by the anterior, posterior and middle cerebral arteries. The actual blood stream blockage/restriction site can be located far away from the infarcts. Watershed locations are those border-zone regions in the brain supplied by the major cerebral arteries where blood supply is decreased. Watershed strokes are a concern because they comprise approximately 10% of all ischemic stroke cases. The watershed zones themselves are particularly susceptible to infarction from global ischemia as the distal nature of the vasculature predisposes these areas to be most sensitive to profound hypoperfusion.
Brain ischemia is a condition in which there is insufficient bloodflow to the brain to meet metabolic demand. This leads to poor oxygen supply or cerebral hypoxia and thus leads to the death of brain tissue or cerebral infarction/ischemic stroke. It is a sub-type of stroke along with subarachnoid hemorrhage and intracerebral hemorrhage.
Animal models of ischemic stroke are procedures inducing cerebral ischemia. The aim is the study of basic processes or potential therapeutic interventions in this disease, and the extension of the pathophysiological knowledge on and/or the improvement of medical treatment of human ischemic stroke. Ischemic stroke has a complex pathophysiology involving the interplay of many different cells and tissues such as neurons, glia, endothelium, and the immune system. These events cannot be mimicked satisfactorily in vitro yet. Thus a large portion of stroke research is conducted on animals.

Ischemic colitis is a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply. Although uncommon in the general population, ischemic colitis occurs with greater frequency in the elderly, and is the most common form of bowel ischemia. Causes of the reduced blood flow can include changes in the systemic circulation or local factors such as constriction of blood vessels or a blood clot. In most cases, no specific cause can be identified.

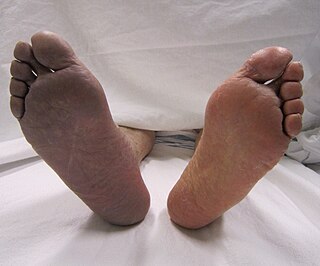
Intestinal ischemia is a medical condition in which injury to the large or small intestine occurs due to not enough blood supply. It can come on suddenly, known as acute intestinal ischemia, or gradually, known as chronic intestinal ischemia. The acute form of the disease often presents with sudden severe abdominal pain and is associated with a high risk of death. The chronic form typically presents more gradually with abdominal pain after eating, unintentional weight loss, vomiting, and fear of eating.

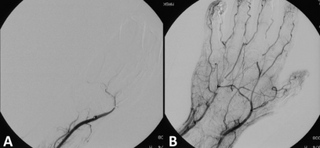
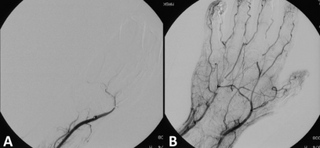
Arterial embolism is a sudden interruption of blood flow to an organ or body part due to an embolus adhering to the wall of an artery blocking the flow of blood, the major type of embolus being a blood clot (thromboembolism). Sometimes, pulmonary embolism is classified as arterial embolism as well, in the sense that the clot follows the pulmonary artery carrying deoxygenated blood away from the heart. However, pulmonary embolism is generally classified as a form of venous embolism, because the embolus forms in veins. Arterial embolism is the major cause of infarction.

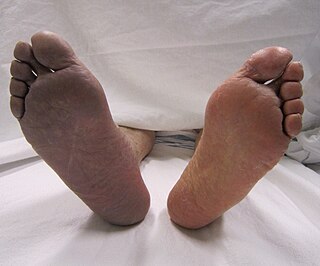
Arterial occlusion is a condition involving partial or complete blockage of blood flow through an artery. Arteries are blood vessels that carry oxygenated blood to body tissues. An occlusion of arteries disrupts oxygen and blood supply to tissues, leading to ischemia. Depending on the extent of ischemia, symptoms of arterial occlusion range from simple soreness and pain that can be relieved with rest, to a lack of sensation or paralysis that could require amputation.