Related Research Articles

Raigmore Hospital is a health facility located in Inverness, Scotland. It serves patients from the local area as well providing specialist services to patients from across the Highland area. It is a teaching hospital, educating a range of healthcare professionals in association with the Universities of Aberdeen and Stirling. It is managed by NHS Highland.
Sir Bruce Edward Keogh, KBE, FRCS, FRCP is a Zimbabwean-born British surgeon who specialises in cardiac surgery. He was Medical Director of the National Health Service in England from 2007 and National Medical Director of the NHS Commissioning Board from 2013 until his retirement early in 2018. He is Chair of Birmingham Women's and Children's NHS Foundation Trust.

The Scottish Ambulance Service is part of NHS Scotland, which serves all of Scotland's population., The Scottish Ambulance Service is governed by a special health board and is funded directly by the Health and Social Care Directorates of the Scottish Government.

NHS Scotland, sometimes styled NHSScotland, is the publicly funded healthcare system in Scotland, and one of the four systems which make up the National Health Service in the United Kingdom. It operates fourteen territorial NHS boards across Scotland, seven special non-geographic health boards and NHS Health Scotland.

The name National Health Service (NHS) is used to refer to the three public health services of England, Scotland and Wales, individually or collectively. Northern Ireland is known as 'Health and Social Care' to promote its dual integration of health and social services.
John Alexander Dewar, 1st Baron Forteviot was a Scottish businessman, elder son of the founder of Dewar's Scotch Whisky and a Liberal Member of Parliament.
Dame Jacqueline Docherty, DBE is a British nursing administrator and medical professional, who was Chief Executive of West Middlesex University Hospital in February 2009 until its merger with Chelsea and Westminster Hospital NHS Foundation Trust, having previously served as Director of Nursing, Director of Operations and Deputy Chief Executive at King's College Hospital, London.

Emergency medical services in the United Kingdom provide emergency care to people with acute illness or injury and are predominantly provided free at the point of use by the four National Health Services of England, Scotland, Wales, and Northern Ireland. Emergency care including ambulance and emergency department treatment is only free to UK Nationals and a charge may be made to those not entitled to free NHS Care.

Health care in the United Kingdom is a devolved matter, with England, Northern Ireland, Scotland and Wales each having their own systems of publicly funded healthcare, funded by and accountable to separate governments and parliaments, together with smaller private sector and voluntary provision. As a result of each country having different policies and priorities, a variety of differences now exist between these systems.

The National Health Service Act 1946 came into effect on 5 July 1948 and created the National Health Service in England and Wales. Though the title 'National Health Service' implies a single health service for the United Kingdom, in reality one NHS was created for England and Wales accountable to the Secretary of State for Health, with a separate NHS created for Scotland accountable to the Secretary of State for Scotland by the passage of the National Health Service (Scotland) Act 1947. Similar health services in Northern Ireland were created by the Northern Ireland Parliament through the Health Services Act 1948.
The rural general hospital is a concept that has been pioneered in the National Health Service in Scotland. A rural general hospital is a small hospital, similar to a district general hospital, but where a specific model of training and staffing allows provision of specific healthcare services to a population in area which is remote and rural.

The Mackinnon Memorial Hospital, also known as Broadford Hospital, is a community hospital, located in the village of Broadford on the Isle of Skye. It is managed by NHS Highland.

The National Health Service (NHS) is the publicly funded healthcare system in England, and one of the four National Health Service systems in the United Kingdom. It is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde. Primarily funded by the government from general taxation, and overseen by the Department of Health and Social Care, the NHS provides healthcare to all legal English residents and residents from other regions of the UK, with most services free at the point of use. Some services, such as emergency treatment and treatment of infectious diseases, are free for most people, including visitors.

Healthcare in Scotland is mainly provided by Scotland's public health service, NHS Scotland. It provides healthcare to all permanent residents free at the point of need and paid for from general taxation. Health is a matter that is devolved, and considerable differences have developed between the public healthcare systems in the different countries of the United Kingdom. Though the public system dominates healthcare provision, private healthcare and a wide variety of alternative and complementary treatments are available for those willing and able to pay.

The National Health Service (NHS) is the umbrella term for the publicly-funded healthcare systems of the United Kingdom (UK). Since 1948 it has been funded out of general taxation. It is made up of the four separate systems of the four countries of the UK: The National Health Service in England, NHS Scotland, NHS Wales, and Health and Social Care in Northern Ireland. They were established together in 1948 as one of the major social reforms following the Second World War. The founding principles were that services should be comprehensive, universal and free at the point of delivery. Each service provides a comprehensive range of health services, free at the point of use for people ordinarily resident in the United Kingdom, apart from dental treatment and optical care. In England, NHS patients have to pay prescription charges with a range of exemptions from these charges.
NHS Scotland is the publicly funded healthcare systems in Scotland. It was founded by the National Health Service (Scotland) Act 1947 and was launched on 5 July 1948, under the control of the Secretary of State for Scotland. As a result of the Scotland Act 1998, control over NHS Scotland transferred to the Scottish Government and Parliament in 1999.
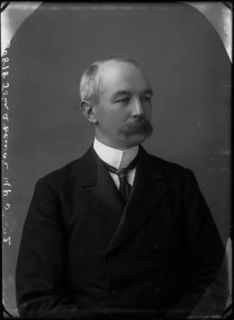
The Report of the Highlands and Islands Medical Service Committee or the Dewar Report was published in 1912 and named after its chair, Sir John Dewar. The report presented a vivid description of the social landscape of the time and highlighted the desperate state of medical provision to the population, particularly in the rural areas of the Highlands and Islands of Scotland. The report recommended setting up a new, centrally planned provision of care that within 20 years transformed medical services to the area. This organisation, the Highlands and Islands Medical Service was widely cited in the Cathcart Report and acted as a working blueprint for the NHS in Scotland. The report is written in clear language and many of its findings continue to have relevance to how medical services are planned and financed in Scotland and beyond.
The King Edward VII Memorial Hospital in Stanley, Falkland Islands is the base for the Falkland Islands Government Health Service. There is a hospital of the same name in Bermuda.
Sir Lewis Duthie Ritchie OBE FRSE FRCSE FRCPE FRCPSG FRCPG FFPH FBCS FRSA CEng (Computing) CITP is a Scottish medical doctor who worked as a general practitioner (GP) and medical researcher. He is the James Mackenzie Professor of General Practice at the University of Aberdeen and holds honorary professorships at the University of Edinburgh and the University of the Highlands and Islands.
Roger McNeill (1853–1924) was a Scottish doctor of public health who was pivotal in bringing about changes to healthcare in the Highlands and Islands.
References
- ↑ "Highlands and Islands Medical Service (HIMS)". ournhsscotland.com. NHS Scotland. Archived from the original on 5 March 2016. Retrieved 12 January 2015.
- ↑ "Archived copy". Archived from the original on 6 December 2014. Retrieved 4 December 2014.CS1 maint: archived copy as title (link)
- ↑ Scottish Board of Health. Consultative Council on Medical and Allied Services. Interim report. A Scheme of Medical Service for Scotland. Cmd. 1039 (Edinburgh, 1920)
- ↑ Scottish Health Services Report ("Cathcart Report") 1935/6 Cmb 5208
- ↑ "Archived copy" (PDF). Archived (PDF) from the original on 30 July 2017. Retrieved 3 March 2013.CS1 maint: archived copy as title (link)