Related Research Articles

Major depressive disorder (MDD), also known as clinical depression, is a mental disorder characterized by at least two weeks of pervasive low mood, low self-esteem, and loss of interest or pleasure in normally enjoyable activities. Introduced by a group of US clinicians in the mid-1970s, the term was adopted by the American Psychiatric Association for this symptom cluster under mood disorders in the 1980 version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), and has become widely used since.

Electroconvulsive therapy (ECT) or electroshock therapy (EST) is a psychiatric treatment where a generalized seizure is electrically induced to manage refractory mental disorders. Typically, 70 to 120 volts are applied externally to the patient's head, resulting in approximately 800 milliamperes of direct current passing between the electrodes, for a duration of 100 milliseconds to 6 seconds, either from temple to temple or from front to back of one side of the head. However, only about 1% of the electrical current crosses the bony skull into the brain because skull impedance is about 100 times higher than skin impedance.
A psychiatric or psychotropic medication is a psychoactive drug taken to exert an effect on the chemical makeup of the brain and nervous system. Thus, these medications are used to treat mental illnesses. These medications are typically made of synthetic chemical compounds and are usually prescribed in psychiatric settings, potentially involuntarily during commitment. Since the mid-20th century, such medications have been leading treatments for a broad range of mental disorders and have decreased the need for long-term hospitalization, thereby lowering the cost of mental health care. The recidivism or rehospitalization of the mentally ill is at a high rate in many countries, and the reasons for the relapses are under research.
Schizoaffective disorder is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis requires symptoms of both schizophrenia and a mood disorder: either bipolar disorder or depression. The main criterion is the presence of psychotic symptoms for at least two weeks without any mood symptoms. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, bipolar I disorder, schizophreniform disorder, or schizophrenia. This is a problem as treatment and prognosis differ greatly for most of these diagnoses.
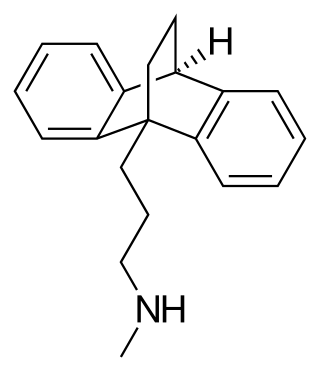
Maprotiline, sold under the brand name Ludiomil among others, is a tetracyclic antidepressant (TeCA) that is used in the treatment of depression. It may alternatively be classified as a tricyclic antidepressant (TCA), specifically a secondary amine. In terms of its chemistry and pharmacology, maprotiline is closely related to such-other secondary-amine TCAs as nortriptyline and protriptyline and has similar effects to them, albeit with more distinct anxiolytic effects. Additionally, whereas protriptyline tends to be somewhat more stimulating and in any case is distinctly more-or-less non-sedating, mild degrees of sedation may be experienced with maprotiline.
Peter Roger Breggin is an American psychiatrist and critic of shock treatment and psychiatric medication and COVID-19 response. In his books, he advocates replacing psychiatry's use of drugs and electroconvulsive therapy with psychotherapy, education, empathy, love, and broader human services.
Biological psychiatry or biopsychiatry is an approach to psychiatry that aims to understand mental disorder in terms of the biological function of the nervous system. It is interdisciplinary in its approach and draws on sciences such as neuroscience, psychopharmacology, biochemistry, genetics, epigenetics and physiology to investigate the biological bases of behavior and psychopathology. Biopsychiatry is the branch of medicine which deals with the study of the biological function of the nervous system in mental disorders.
Treatment-resistant depression is a term used in psychiatry to describe people with major depressive disorder (MDD) who do not respond adequately to a course of appropriate antidepressant medication within a certain time. Definitions of treatment-resistant depression vary, and they do not include a resistance to psychological therapies. Inadequate response has most commonly been defined as less than 50% reduction in depressive symptoms following treatment with at least one antidepressant medication, although definitions vary widely. Some other factors that may contribute to inadequate treatment are: a history of repeated or severe adverse childhood experiences, early discontinuation of treatment, insufficient dosage of medication, patient noncompliance, misdiagnosis, cognitive impairment, low income and other socio-economic variables, and concurrent medical conditions, including comorbid psychiatric disorders. Cases of treatment-resistant depression may also be referred to by which medications people with treatment-resistant depression are resistant to. In treatment-resistant depression adding further treatments such as psychotherapy, lithium, or aripiprazole is weakly supported as of 2019.
A major depressive episode (MDE) is a period characterized by symptoms of major depressive disorder. Those affected primarily exhibit a depressive mood for at least two weeks or more, and a loss of interest or pleasure in everyday activities. Other symptoms can include feelings of emptiness, hopelessness, anxiety, worthlessness, guilt, irritability, changes in appetite, difficulties in concentration, difficulties remembering details, making decisions, and thoughts of suicide. Insomnia or hypersomnia and aches, pains, or digestive problems that are resistant to treatment may also be present.
The emphasis of the treatment of bipolar disorder is on effective management of the long-term course of the illness, which can involve treatment of emergent symptoms. Treatment methods include pharmacological and psychological techniques.
Mental disorders are classified as a psychological condition marked primarily by sufficient disorganization of personality, mind, and emotions to seriously impair the normal psychological and often social functioning of the individual. Individuals diagnosed with certain mental disorders can be unable to function normally in society. Mental disorders may consist of several affective, behavioral, cognitive and perceptual components. The acknowledgement and understanding of mental health conditions has changed over time and across cultures. There are still variations in the definition, classification, and treatment of mental disorders.

Waxy flexibility is one of the twelve symptoms that can lead to the diagnosis of catatonia. It is a psychomotor symptom that results in a decreased response to stimuli and a tendency to remain in an immobile posture. If one were to move the arm of someone with waxy flexibility, the patient would keep that arm where it had been positioned until moved again as if positioning malleable wax. Attempts to reposition the patient are met by "slight, even resistance".
Electroconvulsive therapy is a controversial psychiatric treatment in which seizures are induced with electricity. ECT was first used in the United Kingdom in 1939 and, although its use has been declining for several decades, it was still given to about 11,000 people a year in the early 2000s.
The following outline is provided as an overview of and topical guide to abnormal psychology:
Management of depression is the treatment of depression that may involve a number of different therapies: medications, behavior therapy, psychotherapy, and medical devices.
Late-life depression refers to depression occurring in older adults and has diverse presentations, including as a recurrence of early-onset depression, a new diagnosis of late-onset depression, and a mood disorder resulting from a separate medical condition, substance use, or medication regimen. Research regarding late-life depression often focuses on late-onset depression, which is defined as a major depressive episode occurring for the first time in an older person.

Melancholic depression, or depression with melancholic features, is a DSM-IV and DSM-5 specifier of depressive disorders. The specifier is used to distinguish clinically relevant subsets of causes and symptoms that have the potential to influence treatment.
Schizophrenia is a primary psychotic disorder, whereas, bipolar disorder is a primary mood disorder which can also involve psychosis. Both schizophrenia and bipolar disorder are characterized as critical psychiatric disorders in the Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5). However, because of some similar symptoms, differentiating between the two can sometimes be difficult; indeed, there is an intermediate diagnosis termed schizoaffective disorder.
Musical hallucinations describes a neurological disorder in which the patient will hallucinate songs, tunes, instruments and melodies. The source of these hallucinations are derived from underlying psychotic illness or hearing impairment. These hallucinations are often rare and are followed by mental decline. A majority of patients who have symptoms of musical hallucinations are older and have onset conditions predisposing them to the disease. While there is no set form of treatment, research has discovered medications and alternative therapies to be successful in alleviating the hallucinations.
Psychiatry is, and has historically been, viewed as controversial by those under its care, as well as sociologists and psychiatrists themselves. There are a variety of reasons cited for this controversy, including the subjectivity of diagnosis, the use of diagnosis and treatment for social and political control including detaining citizens and treating them without consent, the side effects of treatments such as electroconvulsive therapy, antipsychotics and historical procedures like the lobotomy and other forms of psychosurgery or insulin shock therapy, and the history of racism within the profession in the United States.
References
- 1 2 3 4 5 6 7 8 Kavanagh, Adam; McLoughlin, Declan (November 2009). "Electroconvulsive Therapy and Nursing Care". British Journal of Nursing. 18 (22): 1370–1377. doi:10.12968/bjon.2009.18.22.45564. PMID 20081692.
- 1 2 3 4 5 Saleem, Nida; Rauf, Shahzad (August 2018). "Efficacy of Electroconvulsive Therapy in Treatment Resistant Depression". Pakistan Armed Forces Medical Journal. 68: 969–974 – via Academic Search Complete.
- 1 2 3 Cyrzyk, Thomas (April 2013). "Electroconvulsive therapy: why it is still controversial". Mental Health Practice. 16 (7): 22–27. doi:10.7748/mhp2013.04.16.7.22.e769.
- 1 2 3 4 5 Kellner, Charles (January 2011). "Electroconvulsive Therapy The Second Most Controversial Medical Procedure". Psychiatric Times. 28: 41–47 – via CINAHL Complete.
- 1 2 Srienc, Anja; NARANG, PUNEET (April 2018). "Is Electroconvulsive Therapy a Treatment for Depression Following Traumatic Brain Injury". Innovations in Clinical Neuroscience. 15 (3–4): 43–46. PMC 5906090 . PMID 29707426.
- 1 2 3 4 5 Sharma, Natasha; Ghai, Sandhya (2017). "Knowledge and attitude of nursing students toward electroconvulsive therapy". Journal of Neurosciences in Rural Practice. 8: 7–12 – via Directory of Open Access Journals.
- 1 2 3 4 5 6 7 8 9 10 Piotrowski, Nancy (2013). "Shock Therapy". Magill's Medical Guide– via Research Starters.
- 1 2 3 Sharpley, Christopher (June 2011). "Antidepressants in counseling psychology-Relevance, effectiveness and implications for practice". Counselling Psychology Quarterly. 24 (2): 139–156. doi:10.1080/09515070.2011.589245. S2CID 143791415.