Related Research Articles

Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage."

An itch is a sensation that causes a strong desire or reflex to scratch. Itches have resisted many attempts to be classified as any one type of sensory experience. Itches have many similarities to pain, and while both are unpleasant sensory experiences, their behavioral response patterns are different. Pain creates a withdrawal reflex, whereas itches leads to a scratch reflex.

A nociceptor is a sensory neuron that responds to damaging or potentially damaging stimuli by sending "possible threat" signals to the spinal cord and the brain. The brain creates the sensation of pain to direct attention to the body part, so the threat can be mitigated; this process is called nociception.

The threshold of pain or pain threshold is the point along a curve of increasing perception of a stimulus at which pain begins to be felt. It is an entirely subjective phenomenon. A distinction must be maintained between the stimulus and the person's or animal's resulting pain perception. Although an IASP document defines "pain threshold" as "the minimum intensity of a stimulus that is perceived as painful", it then goes on to say that:
Traditionally the threshold has often been defined, as we defined it formerly, as the least stimulus intensity at which a subject perceives pain. Properly defined, the threshold is really the experience of the patient, whereas the intensity measured is an external event. It has been common usage for most pain research workers to define the threshold in terms of the stimulus, and that should be avoided ... The stimulus is not pain (q.v.) and cannot be a measure of pain.

Hyperalgesia is an abnormally increased sensitivity to pain, which may be caused by damage to nociceptors or peripheral nerves and can cause hypersensitivity to stimulus. Prostaglandins E and F are largely responsible for sensitizing the nociceptors. Temporary increased sensitivity to pain also occurs as part of sickness behavior, the evolved response to infection.
Neuralgia is pain in the distribution of a nerve or nerves, as in intercostal neuralgia, trigeminal neuralgia, and glossopharyngeal neuralgia.

Allodynia is a condition in which pain is caused by a stimulus that does not normally elicit pain. For example, sunburn can cause temporary allodynia, so that usually painless stimuli, such as wearing clothing or running cold or warm water over it, can be very painful. It is different from hyperalgesia, an exaggerated response from a normally painful stimulus. The term comes from Ancient Greek άλλος (állos) 'other' and οδύνη (odúnē) 'pain'.
Hyperesthesia is a condition that involves an abnormal increase in sensitivity to stimuli of the senses. Stimuli of the senses can include sound that one hears, foods that one tastes, textures that one feels, and so forth. Increased touch sensitivity is referred to as "tactile hyperesthesia", and increased sound sensitivity is called "auditory hyperesthesia". In the context of pain, hyperaesthesia can refer to an increase in sensitivity where there is both allodynia and hyperalgesia.
Dysesthesia is an unpleasant, abnormal sense of touch. Its etymology comes from the Greek word "dys," meaning "bad," and "aesthesis," which means "sensation". It often presents as pain but may also present as an inappropriate, but not discomforting, sensation. It is caused by lesions of the nervous system, peripheral or central, and it involves sensations, whether spontaneous or evoked, such as burning, wetness, itching, electric shock, and pins and needles. Dysesthesia can include sensations in any bodily tissue, including most often the mouth, scalp, skin, or legs.

Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A and B are myelinated. Group C fibers include postganglionic fibers in the autonomic nervous system (ANS), and nerve fibers at the dorsal roots. These fibers carry sensory information.

Transient receptor potential cation channel subfamily M (melastatin) member 8 (TRPM8), also known as the cold and menthol receptor 1 (CMR1), is a protein that in humans is encoded by the TRPM8 gene. The TRPM8 channel is the primary molecular transducer of cold somatosensation in humans. In addition, mints can desensitize a region through the activation of TRPM8 receptors.
Dejerine–Roussy syndrome or thalamic pain syndrome is a condition developed after a thalamic stroke, a stroke causing damage to the thalamus. Ischemic strokes and hemorrhagic strokes can cause lesioning in the thalamus. As initial stroke symptoms dissipate, an imbalance in sensation causes these later syndromes, characterizing Dejerine–Roussy syndrome. Although some treatments exist, they are often expensive, chemically based, invasive, and only treat patients for some time before they need more treatment, called "refractory treatment".

Nav1.8 is a sodium ion channel subtype that in humans is encoded by the SCN10A gene.
Mechanosensation is the transduction of mechanical stimuli into neural signals. Mechanosensation provides the basis for the senses of light touch, hearing, proprioception, and pain. Mechanoreceptors found in the skin, called cutaneous mechanoreceptors, are responsible for the sense of touch. Tiny cells in the inner ear, called hair cells, are responsible for hearing and balance. States of neuropathic pain, such as hyperalgesia and allodynia, are also directly related to mechanosensation. A wide array of elements are involved in the process of mechanosensation, many of which are still not fully understood.

The wide dynamic range (WDR) neuron was first discovered by Mendell in 1966. Early studies of this neuron established what is known as the gate control theory of pain. The basic concept is that non-painful stimuli block the pathways for painful stimuli, inhibiting possible painful responses. This theory was supported by the fact that WDR neurons are responsible for responses to both painful and non-painful stimuli, and the idea that these neurons could not produce more than one of these responses simultaneously. WDR neurons respond to all types of somatosensory stimuli, make up the majority of the neurons found in the posterior grey column, and have the ability to produce long range responses including those responsible for pain and itch.
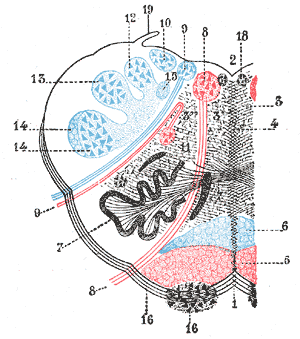
The rostral ventromedial medulla (RVM), or ventromedial nucleus of the spinal cord, is a group of neurons located close to the midline on the floor of the medulla oblongata. The rostral ventromedial medulla sends descending inhibitory and excitatory fibers to the dorsal horn spinal cord neurons. There are 3 categories of neurons in the RVM: on-cells, off-cells, and neutral cells. They are characterized by their response to nociceptive input. Off-cells show a transitory decrease in firing rate right before a nociceptive reflex, and are theorized to be inhibitory. Activation of off-cells, either by morphine or by any other means, results in antinociception. On-cells show a burst of activity immediately preceding nociceptive input, and are theorized to be contributing to the excitatory drive. Neutral cells show no response to nociceptive input.
Ocular neuropathic pain, also called corneal neuralgia, is a spectrum of disorders of ocular pain which are caused by damage or disease affecting the nerves. Ocular neuropathic pain is frequently associated with damaged or dysfunctional corneal nerves, but the condition can also be caused by peripheral or centralized sensitization. The condition shares some characteristics with somatic neuropathic pain in that it is similarly associated with abnormal sensations (dysesthesia) or pain from normally non-painful stimuli (allodynia), but until recent years has been poorly understood by the medical community, and frequently dismissed by ophthalmologists who were not trained to identify neuropathic pain as a source of unexplained eye pain beyond objective findings noted on slit-lamp examination.
Peripheral mononeuropathy is a nerve related disease where a single nerve, that is used to transport messages from the brain to the peripheral body, is diseased or damaged. Peripheral neuropathy is a general term that indicates any disorder of the peripheral nervous system. The name of the disorder itself can be broken down in order to understand this better; peripheral: in regard to peripheral neuropathy, refers to outside of the brain and spinal cord; neuro: means nerve related; -pathy; means disease. Peripheral mononeuropathy is a disorder that links to Peripheral Neuropathy, as it only effects a single peripheral nerve rather than several damaged or diseased nerves throughout the body. Healthy peripheral nerves are able to “carry messages from the brain and spinal cord to muscles, organs, and other body tissues”.

Nociplastic pain, also known as central sensitisation, is the consensus semantic term used by medical researchers to describe a third category of pain that is mechanistically distinct from nociceptive pain, due to inflammation and tissue damage, and neuropathic pain, due to nerve damage. It may occur in combination with the other types of pain or in isolation. Its location may be generalised or multifocal and it can be more intense than would be expected from any associated physical cause.
References
- ↑ Jensen, T. S. (1996). Mechanisms of neuropathic pain. In J. N. Campbell (Ed.), Pain, 1996, an updated review. (pp. 77-86). Seattle: IASP Press
- ↑ (I.A.S.P, 1986). Pain Supplement 3: Classification of Chronic Pain, Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. Amsterdam: Elsevier.