Colorectal cancer (CRC), also known as bowel cancer, colon cancer, or rectal cancer, is the development of cancer from the colon or rectum. Signs and symptoms may include blood in the stool, a change in bowel movements, weight loss, and fatigue. Most colorectal cancers are due to old age and lifestyle factors, with only a small number of cases due to underlying genetic disorders. Risk factors include diet, obesity, smoking, and lack of physical activity. Dietary factors that increase the risk include red meat, processed meat, and alcohol. Another risk factor is inflammatory bowel disease, which includes Crohn's disease and ulcerative colitis. Some of the inherited genetic disorders that can cause colorectal cancer include familial adenomatous polyposis and hereditary non-polyposis colon cancer; however, these represent less than 5% of cases. It typically starts as a benign tumor, often in the form of a polyp, which over time becomes cancerous.

A Krukenberg tumor refers to a malignancy in the ovary that metastasized from a primary site, classically the gastrointestinal tract, although it can arise in other tissues such as the breast. Gastric adenocarcinoma, especially at the pylorus, is the most common source. Krukenberg tumors are often found in both ovaries, consistent with its metastatic nature.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

Pseudomyxoma peritonei (PMP) is a clinical condition caused by cancerous cells that produce abundant mucin or gelatinous ascites. The tumors cause fibrosis of tissues and impede digestion or organ function, and if left untreated, the tumors and mucin they produce will fill the abdominal cavity. This will result in compression of organs and will destroy the function of the colon, small intestine, stomach, or other organs. Prognosis with treatment in many cases is optimistic, but the disease is lethal if untreated, with death occurring via cachexia, bowel obstruction, or other types of complications.

Desmoplastic small-round-cell tumor (DSRCT) is an aggressive and rare cancer that primarily occurs as masses in the abdomen. Other areas affected may include the lymph nodes, the lining of the abdomen, diaphragm, spleen, liver, chest wall, skull, spinal cord, large intestine, small intestine, bladder, brain, lungs, testicles, ovaries, and the pelvis. Reported sites of metastatic spread include the liver, lungs, lymph nodes, brain, skull, and bones. It is characterized by the EWS-WT1 fusion protein.

Omental cake is a radiologic sign indicative of an abnormally thickened greater omentum. It refers to infiltration of the normal omental structure by other types of soft-tissue or chronic inflammation resulting in a thickened, or cake-like appearance.
Carcinosis, or carcinomatosis, is disseminated cancer, forms of metastasis, whether used generally or in specific patterns of spread.
Hepatic arterial infusion (HAI) is a medical procedure that delivers chemotherapy directly to the liver. The procedure, mostly used in combination with systemic chemotherapy, plays a role in the treatment of liver metastases in patients with colorectal cancer (CRC). Although surgical resection remains the standard of care for these liver metastases, majority of patients have lesions that are unresectable.
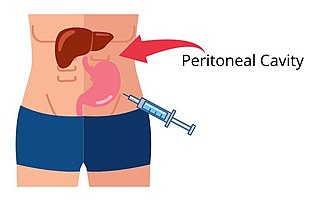
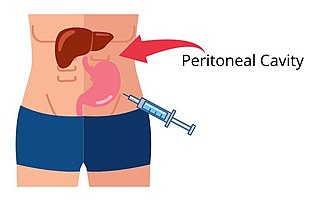
Intraperitoneal injection or IP injection is the injection of a substance into the peritoneum. It is more often applied to non-human animals than to humans. In general, it is preferred when large amounts of blood replacement fluids are needed or when low blood pressure or other problems prevent the use of a suitable blood vessel for intravenous injection.

Peritoneal mesothelioma is the name given to the cancer that attacks the lining of the abdomen. This type of cancer affects the lining that protects the contents of the abdomen and which also provides a lubricating fluid to enable the organs to move and work properly.
Hyperthermic intrathoracic chemotherapy (HITOC) is part of a surgical strategy employed in the treatment of various pleural malignancies. The pleura in this situation could be considered to include the surface linings of the chest wall, lungs, mediastinum, and diaphragm. HITOC is the chest counterpart of HIPEC. Traditionally used in the treatment of malignant mesothelioma, a primary malignancy of the pleura, this modality has recently been evaluated in the treatment of secondary pleural malignancies.
Cytoreductive surgery (CRS) is a surgical procedure that aims to reduce the amount of cancer cells in the abdominal cavity for patients with tumors that have spread intraabdominally. It is often used to treat ovarian cancer but can also be used for other abdominal malignancies.

Farrer Park Hospital is a private tertiary healthcare institution in Farrer Park, Singapore. Located above the Farrer Park MRT station at the Connexion building, the hospital has a capacity of 220 beds across four inpatient suites and 18 operating theaters including major surgery, cardiovascular and endoscopic suites. It is interconnected with the Farrer Park Medical Centre, where there are 10 floors of suites for over 200 medical specialists, as well as One Farrer Hotel.

Peritoneal carcinomatosis (PC) is intraperitoneal dissemination (carcinosis) of any form of cancer that does not originate from the peritoneum itself. PC is most commonly seen in abdominopelvic malignancies. Computed tomography (CT) is particularly important for detailed preoperative assessment and evaluation of the radiological Peritoneal Cancer Index (PCI).
Paul Hendrick Sugarbaker is an American surgeon at the Washington Cancer Institute. He is known for developments in surgical oncology of the abdomen, including cytoreductive surgery followed by hyperthermic intraperitoneal chemotherapy, or HIPEC, a treatment alternately referred to as the Sugarbaker Procedure.
Juan José Segura-Sampedro MBE is a Spanish surgeon and researcher at Son Espases University Hospital in Mallorca, Spain, and adjunct professor of surgery at University of the Balearic Islands. He is best known for his research in major trauma, focused on the balconing phenomenon and a preventive campaign in collaboration with the British Foreign Office.
Ovarian germ cell tumors (OGCTs) are heterogeneous tumors that are derived from the primitive germ cells of the embryonic gonad, which accounts for about 2.6% of all ovarian malignancies. There are four main types of OGCTs, namely dysgerminomas, yolk sac tumor, teratoma, and choriocarcinoma.
Andrea A. Hayes Dixon is an American surgeon. She was the first pediatric surgeon to perform a high-risk, life-saving procedure in children with a rare form of cancer and developed the first orthotropic xenograft model of metastatic Ewing's sarcoma. In 2002, she became the first African American female pediatric surgeon board-certified in the United States.
Gilles Freyer is a French professor, oncologist and medical professional who has specialised in the field of gynaecological cancers. He is currently head of the Department of Medical Oncology and Vice-Dean of the University of Lyon. He is also the current Medical Director of the Cancer Institute of the Hospices Civils de Lyon. He is known for having been the President of the cooperative group GINECO from 2013. He was also a member of the International Scientific Committee of INCa. Professor Freyer is also known for being the President of the Monaco Age Oncologie and the Co-President of the Biennale Monégasque de Cancérologie.
Somashekhar SP is an Indian robotic surgeon, author and chairman of medical advisory board at Aster DM Healthcare - GCC & India. He is also the global director of Aster International Institute of Oncology in GCC & India. He is the president of the Association of Breast Surgeons of India, editor in chief of the IJGO Springer Indian Journal of Gynec Oncology and council member of The Association of Surgeons of India. He is also the editor of Annals of Breast Diseases.