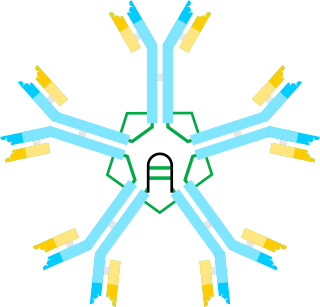
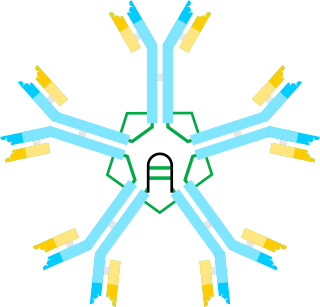
Immunoglobulin G (IgG) is a type of antibody. Representing approximately 75% of serum antibodies in humans, IgG is the most common type of antibody found in blood circulation. IgG molecules are created and released by plasma B cells. Each IgG antibody has two paratopes.

Immunoglobulin A is an antibody that plays a role in the immune function of mucous membranes. The amount of IgA produced in association with mucosal membranes is greater than all other types of antibody combined. In absolute terms, between three and five grams are secreted into the intestinal lumen each day. This represents up to 15% of total immunoglobulins produced throughout the body.
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. Most cases are acquired ("secondary") due to extrinsic factors that affect the patient's immune system. Examples of these extrinsic factors include HIV infection and environmental factors, such as nutrition. Immunocompromisation may also be due to genetic diseases/flaws such as SCID.

X-linked agammaglobulinemia (XLA) is a rare genetic disorder discovered in 1952 that affects the body's ability to fight infection. As the form of agammaglobulinemia that is X-linked, it is much more common in males. In people with XLA, the white blood cell formation process does not generate mature B cells, which manifests as a complete or near-complete lack of proteins called gamma globulins, including antibodies, in their bloodstream. B cells are part of the immune system and normally manufacture antibodies, which defend the body from infections by sustaining a humoral immunity response. Patients with untreated XLA are prone to develop serious and even fatal infections. A mutation occurs at the Bruton's tyrosine kinase (Btk) gene that leads to a severe block in B cell development and a reduced immunoglobulin production in the serum. Btk is particularly responsible for mediating B cell development and maturation through a signaling effect on the B cell receptor BCR. Patients typically present in early childhood with recurrent infections, in particular with extracellular, encapsulated bacteria. XLA is deemed to have a relatively low incidence of disease, with an occurrence rate of approximately 1 in 200,000 live births and a frequency of about 1 in 100,000 male newborns. It has no ethnic predisposition. XLA is treated by infusion of human antibody. Treatment with pooled gamma globulin cannot restore a functional population of B cells, but it is sufficient to reduce the severity and number of infections due to the passive immunity granted by the exogenous antibodies.
Hypogammaglobulinemia is an immune system disorder in which not enough gamma globulins are produced in the blood. This results in a lower antibody count, which impairs the immune system, increasing risk of infection. Hypogammaglobulinemia may result from a variety of primary genetic immune system defects, such as common variable immunodeficiency, or it may be caused by secondary effects such as medication, blood cancer, or poor nutrition, or loss of gamma globulins in urine, as in nonselective glomerular proteinuria. Patients with hypogammaglobulinemia have reduced immune function; important considerations include avoiding use of live vaccines, and take precautionary measures when traveling to regions with endemic disease or poor sanitation such as receiving immunizations, taking antibiotics abroad, drinking only safe or boiled water, arranging appropriate medical cover in advance of travel, and ensuring continuation of any immunoglobulin infusions needed.
Common variable immunodeficiency (CVID) is an immune disorder characterized by recurrent infections and low antibody levels, specifically in immunoglobulin (Ig) types IgG, IgM, and IgA. Symptoms generally include high susceptibility to foreign invaders, chronic lung disease, and inflammation and infection of the gastrointestinal tract. CVID affects males and females equally. The condition can be found in children or teens but is generally not diagnosed or recognized until adulthood. The average age of diagnosis is between 20 and 50. However, symptoms vary greatly between people. "Variable" refers to the heterogeneous clinical manifestations of this disorder, which include recurrent bacterial infections, increased risk for autoimmune disease and lymphoma, as well as gastrointestinal disease. CVID is a lifelong disease.

Selective immunoglobulin A (IgA) deficiency (SIgAD) is a kind of immunodeficiency, a type of hypogammaglobulinemia. People with this deficiency lack immunoglobulin A (IgA), a type of antibody that protects against infections of the mucous membranes lining the mouth, airways, and digestive tract. It is defined as an undetectable serum IgA level in the presence of normal serum levels of IgG and IgM, in persons older than 4 years. It is the most common of the primary antibody deficiencies. Most such persons remain healthy throughout their lives and are never diagnosed.

Dysgammaglobulinemia is a type of immune disorder characterized by a reduction in some types of gamma globulins, resulting in heightened susceptibility to some infectious diseases where primary immunity is antibody based.
Hyper IgM Syndrome Type 2 is a rare disease. Unlike other hyper-IgM syndromes, Type 2 patients identified thus far did not present with a history of opportunistic infections. One would expect opportunistic infections in any immunodeficiency syndrome. The responsible genetic lesion is in the AICDA gene found at 12p13.
The fifth type of hyper-IgM syndrome has been characterized in three patients from France and Japan. The symptoms are similar to hyper IgM syndrome type 2, but the AICDA gene is intact.
Primary immunodeficiencies are disorders in which part of the body's immune system is missing or does not function normally. To be considered a primary immunodeficiency (PID), the immune deficiency must be inborn, not caused by secondary factors such as other disease, drug treatment, or environmental exposure to toxins. Most primary immunodeficiencies are genetic disorders; the majority are diagnosed in children under the age of one, although milder forms may not be recognized until adulthood. While there are over 430 recognized inborn errors of immunity (IEIs) as of 2019, the vast majority of which are PIDs, most are very rare. About 1 in 500 people in the United States are born with a primary immunodeficiency. Immune deficiencies can result in persistent or recurring infections, auto-inflammatory disorders, tumors, and disorders of various organs. There are currently limited treatments available for these conditions; most are specific to a particular type of PID. Research is currently evaluating the use of stem cell transplants (HSCT) and experimental gene therapies as avenues for treatment in limited subsets of PIDs.

In immunology, antibodies are classified into several types called isotypes or classes. The variable (V) regions near the tip of the antibody can differ from molecule to molecule in countless ways, allowing it to specifically target an antigen . In contrast, the constant (C) regions only occur in a few variants, which define the antibody's class. Antibodies of different classes activate distinct effector mechanisms in response to an antigen . They appear at different stages of an immune response, differ in structural features, and in their location around the body.
Isolated primary immunoglobulin M deficiency is a poorly defined dysgammaglobulinemia characterized by decreased levels of IgM while levels of other immunoglobulins are normal. The immunodeficiency has been associated with some clinical disorders including recurrent infections, atopy, Bloom's syndrome, celiac disease, systemic lupus erythematosus and malignancy, but, surprisingly, SIgMD seems to also occur in asymptomatic individuals. High incidences of recurrent upper respiratory tract infections (77%), asthma (47%) and allergic rhinitis (36%) have also been reported. SIgMD seems to be a particularly rare antibody deficiency with a reported prevalence between 0.03% and 0.1%.

Humoral immune deficiencies are conditions which cause impairment of humoral immunity, which can lead to immunodeficiency. It can be mediated by insufficient number or function of B cells, the plasma cells they differentiate into, or the antibody secreted by the plasma cells. The most common such immunodeficiency is inherited selective IgA deficiency, occurring between 1 in 100 and 1 in 1000 persons, depending on population. They are associated with increased vulnerability to infection, but can be difficult to detect in the absence of infection.
Hyper-IgM syndrome type 3 is a form of hyper IgM syndrome characterized by mutations of the CD40 gene. In this type, Immature B cells cannot receive signal 2 from helper T cells which is necessary to mature into mature B cells.
Hyper-IgM syndrome type 4 is a form of Hyper IgM syndrome which is a defect in class switch recombination downstream of the AICDA gene that does not impair somatic hypermutation.
Thymoma with immunodeficiency is a rare disorder that occurs in adults in whom hypogammaglobulinemia, deficient cell-mediated immunity, and thymoma may develop almost simultaneously. Most reported cases are in Europe, though it occurs globally.

Caspase-8 deficiency (CEDS) is a very rare genetic disorder of the immune system. It is caused by mutations in the CASP8 gene that encodes the protein caspase-8. The disorder is characterized by splenomegaly and lymphadenopathy, in addition to recurrent sinopulmonary infections, recurrent mucocutaneous herpesvirus or other viral infections, and hypogammaglobulinemia. Investigators in the laboratory of Dr. Michael Lenardo at the National Institutes of Health described this condition in two siblings from a consanguineous family in 2002, and several more affected family members have since been identified.
Immunoglobulin therapy is the use of a mixture of antibodies to treat several health conditions. These conditions include primary immunodeficiency, immune thrombocytopenic purpura, chronic inflammatory demyelinating polyneuropathy, Kawasaki disease, certain cases of HIV/AIDS and measles, Guillain-Barré syndrome, and certain other infections when a more specific immunoglobulin is not available. Depending on the formulation it can be given by injection into muscle, a vein, or under the skin. The effects last a few weeks.
Anti-immunoglobulin antibodies are defined as a protein that detects other antibodies from an organism. Specifically, anti-immunoglobulin antibodies are created by B-cells as antibodies to bind to other immunoglobulins. Immunoglobulins have two regions: the constant region and the variable region. The constant region is involved in effector function, while the variable region is involved in recognizing and binding to antigens. Anti-immunoglobulin antibodies may bind to either the variable or constant region of the immunoglobulin. Anti-immunoglobulin antibodies are a type of secondary antibody. They are able to detect primary antibodies through multiple methods such as a Western blot, immunohistochemistry, immunofluorescence staining, flow cytometry, and ELISA.