Cushing's syndrome is a collection of signs and symptoms due to prolonged exposure to glucocorticoids such as cortisol. Signs and symptoms may include high blood pressure, abdominal obesity but with thin arms and legs, reddish stretch marks, a round red face due to facial plethora, a fat lump between the shoulders, weak muscles, weak bones, acne, and fragile skin that heals poorly. Women may have more hair and irregular menstruation. Occasionally there may be changes in mood, headaches, and a chronic feeling of tiredness.

Gigantism, also known as giantism, is a condition characterized by excessive growth and height significantly above average. In humans, this condition is caused by over-production of growth hormone in childhood.
Cushing's disease is one cause of Cushing's syndrome characterised by increased secretion of adrenocorticotropic hormone (ACTH) from the anterior pituitary. This is most often as a result of a pituitary adenoma or due to excess production of hypothalamus CRH that stimulates the synthesis of cortisol by the adrenal glands. Pituitary adenomas are responsible for 80% of endogenous Cushing's syndrome, when excluding Cushing's syndrome from exogenously administered corticosteroids. The equine version of this disease is Pituitary pars intermedia dysfunction.

Proteus syndrome is a rare disorder with a genetic background that can cause tissue overgrowth involving all three embryonic lineages. Patients with Proteus syndrome tend to have an increased risk of embryonic tumor development. The clinical and radiographic symptoms of Proteus syndrome are highly variable, as are its orthopedic manifestations.
In medical or research imaging, an incidental imaging finding is an unanticipated finding which is not related to the original diagnostic inquiry. As with other types of incidental medical findings, they may represent a diagnostic, ethical, and philosophical dilemma because their significance is unclear. While some coincidental findings may lead to beneficial diagnoses, others may lead to overdiagnosis that results in unnecessary testing and treatment, sometimes called the "cascade effect".

Pituitary adenomas are tumors that occur in the pituitary gland. Most pituitary tumors are benign, approximately 35% are invasive and just 0.1% to 0.2% are carcinomas. Pituitary adenomas represent from 10% to 25% of all intracranial neoplasms and the estimated prevalence rate in the general population is approximately 17%.

A craniopharyngioma is a rare type of brain tumor derived from pituitary gland embryonic tissue that occurs most commonly in children, but also affects adults. It may present at any age, even in the prenatal and neonatal periods, but peak incidence rates are childhood-onset at 5–14 years and adult-onset at 50–74 years. People may present with bitemporal inferior quadrantanopia leading to bitemporal hemianopsia, as the tumor may compress the optic chiasm. It has a point prevalence around two per 1,000,000. Craniopharyngiomas are distinct from Rathke's cleft tumours and intrasellar arachnoid cysts.

22q13 deletion syndrome, also known as Phelan–McDermid syndrome (PMS), is a genetic disorder caused by deletions or rearrangements on the q terminal end of chromosome 22. Any abnormal genetic variation in the q13 region that presents with significant manifestations (phenotype) typical of a terminal deletion may be diagnosed as 22q13 deletion syndrome. There is disagreement among researchers as to the exact definition of 22q13 deletion syndrome. The Developmental Synaptopathies Consortium defines PMS as being caused by SHANK3 mutations, a definition that appears to exclude terminal deletions. The requirement to include SHANK3 in the definition is supported by many but not by those who first described 22q13 deletion syndrome.
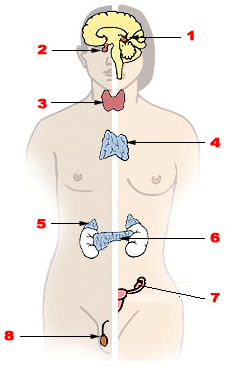
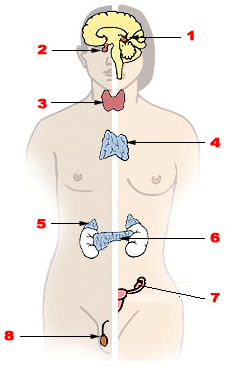
Endocrine diseases are disorders of the endocrine system. The branch of medicine associated with endocrine disorders is known as endocrinology.
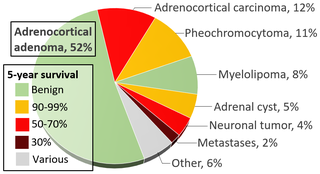
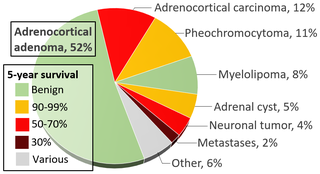
An adrenal tumor or adrenal mass is any benign or malignant neoplasms of the adrenal gland, several of which are notable for their tendency to overproduce endocrine hormones. Adrenal cancer is the presence of malignant adrenal tumors, and includes neuroblastoma, adrenocortical carcinoma and some adrenal pheochromocytomas. Most adrenal pheochromocytomas and all adrenocortical adenomas are benign tumors, which do not metastasize or invade nearby tissues, but may cause significant health problems by unbalancing hormones.

An adrenocortical adenoma or adrenal adenoma is commonly described as a benign neoplasm emerging from the cells that comprise the adrenal cortex. Like most adenomas, the adrenocortical adenoma is considered a benign tumor since the majority of them are non-functioning and asymptomatic. Adrenocortical adenomas are classified as ACTH-independent disorders, and are commonly associated with conditions linked to hyperadrenalism such as Cushing's syndrome (hypercortisolism) or Conn's syndrome (hyperaldosteronism), which is also known as primary aldosteronism. In addition, recent case reports further support the affiliation of adrenocortical adenomas with hyperandrogenism or florid hyperandrogenism which can cause hyperandrogenic hirsutism in females. "Cushing's syndrome" differs from the "Cushing's disease" even though both conditions are induced by hypercortisolism. The term "Cushing's disease" refers specifically to "secondary hypercortisolism" classified as "ACTH-dependent Cushing's syndrome" caused by pituitary adenomas. In contrast, "Cushing's syndrome" refers specifically to "primary hypercortisolism" classified as "ACTH-independent Cushing's syndrome" caused by adrenocortical adenomas.
The exome is composed of all of the exons within the genome, the sequences which, when transcribed, remain within the mature RNA after introns are removed by RNA splicing. This includes untranslated regions of messenger RNA (mRNA), and coding regions. Exome sequencing has proven to be an efficient method of determining the genetic basis of more than two dozen Mendelian or single gene disorders.
Cancer genome sequencing is the whole genome sequencing of a single, homogeneous or heterogeneous group of cancer cells. It is a biochemical laboratory method for the characterization and identification of the DNA or RNA sequences of cancer cell(s).

Exome sequencing, also known as whole exome sequencing (WES), is a genomic technique for sequencing all of the protein-coding regions of genes in a genome. It consists of two steps: the first step is to select only the subset of DNA that encodes proteins. These regions are known as exons—humans have about 180,000 exons, constituting about 1% of the human genome, or approximately 30 million base pairs. The second step is to sequence the exonic DNA using any high-throughput DNA sequencing technology.

Depression, one of the most commonly diagnosed psychiatric disorders, is being diagnosed in increasing numbers in various segments of the population worldwide. Depression in the United States alone affects 17.6 million Americans each year or 1 in 6 people. Depressed patients are at increased risk of type 2 diabetes, cardiovascular disease and suicide. Within the next twenty years depression is expected to become the second leading cause of disability worldwide and the leading cause in high-income nations, including the United States. In approximately 75% of suicides, the individuals had seen a physician within the prior year before their death, 45–66% within the prior month. About a third of those who died by suicide had contact with mental health services in the prior year, a fifth within the preceding month.

Robert C. Green is an American medical geneticist, physician, and public health researcher. He directs the Genomes2People Research Program in translational genomics and health outcomes in the Division of Genetics at Brigham and Women's Hospital and the Broad Institute, and is Director of the Preventive Genomics Clinic at Brigham and Women's Hospital. Research led by Green includes clinical and research aspects of genomic and precision medicine, including the development and disclosure of Alzheimer's disease risk estimates and one of the first prospective studies of direct-to-consumer genetic testing services. He has studied the implementation of medical sequencing in healthy adults, newborns, and active duty military personnel. As of 2020, he is leading the first research collaboration to explore return of genomic results and better understand penetrance in a population-based cohort of underrepresented minorities. He has led the Preventive Genomics Clinic at Brigham and Women's Hospital since its creation in 2019.
Ellen Wright Clayton is an American Rosalind E. Franklin Professor of genetics and chairwoman of the Institute of Medicine Board at the Population Health and Public Health Practice who became a 2013 recipient of the David Rall Medal.
The Undiagnosed Diseases Network (UDN) is a research study that is funded by the National Institutes of Health Common Fund. Its purpose is to bring together clinical and research experts from across the United States to solve the most challenging medical mysteries using advanced technologies.
The Qatar Genome Programme aims to sequence the genomes of 350,000 inhabitants of Qatar. Supported by the Sidra Medical and Research Center, the program is managed by Qatar Genome Committee and wants to eventually offer personalized healthcare in Qatar to its population with advances in genomics. The Qatar Genome Programme published its first genome-wide association study with 45 clinically relevant traits in 2021
Elective genetic and genomic testing are DNA tests performed for an individual who does not have an indication for testing. An elective genetic test analyzes selected sites in the human genome while an elective genomic test analyzes the entire human genome. Some elective genetic and genomic tests require a physician to order the test to ensure that individuals understand the risks and benefits of testing as well as the results. Other DNA-based tests, such as a genealogical DNA test do not require a physician's order. Elective testing is generally not paid for by health insurance companies. With the advent of personalized medicine, also called precision medicine, an increasing number of individuals are undertaking elective genetic and genomic testing.