Dental products are specially fabricated materials, designed for use in dentistry. There are many different types of dental products, and their characteristics vary according to their intended purpose.

A bridge is a fixed dental restoration used to replace one or more missing teeth by joining an artificial tooth definitively to adjacent teeth or dental implants.
Dental restoration, dental fillings, or simply fillings are treatments used to restore the function, integrity, and morphology of missing tooth structure resulting from caries or external trauma as well as to the replacement of such structure supported by dental implants. They are of two broad types—direct and indirect—and are further classified by location and size. A root canal filling, for example, is a restorative technique used to fill the space where the dental pulp normally resides.
Dental sealants are a dental treatment intended to prevent tooth decay. Teeth have recesses on their biting surfaces; the back teeth have fissures (grooves) and some front teeth have cingulum pits. It is these pits and fissures that are most vulnerable to tooth decay because food and bacteria stick in them and because they are hard-to-clean areas. Dental sealants are materials placed in these pits and fissures to fill them in, creating a smooth surface which is easy to clean. Dental sealants are mainly used in children who are at higher risk of tooth decay, and are usually placed as soon as the adult molar teeth come through.

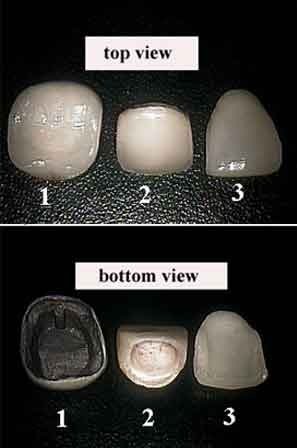
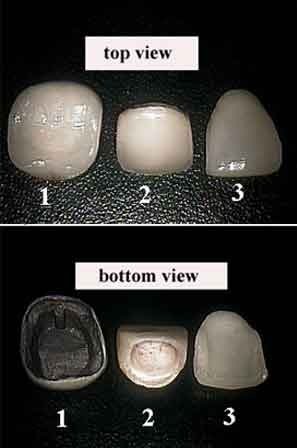
In dentistry, a crown or a dental cap is a type of dental restoration that completely caps or encircles a tooth or dental implant. A crown may be needed when a large dental cavity threatens the health of a tooth. A crown is typically bonded to the tooth by dental cement. They can be made from various materials, which are usually fabricated using indirect methods. Crowns are used to improve the strength or appearance of teeth and to halt deterioration. While beneficial to dental health, the procedure and materials can be costly.

Dental composite resins are dental cements made of synthetic resins. Synthetic resins evolved as restorative materials since they were insoluble, of good tooth-like appearance, insensitive to dehydration, easy to manipulate and inexpensive. Composite resins are most commonly composed of Bis-GMA and other dimethacrylate monomers, a filler material such as silica and in most applications, a photoinitiator. Dimethylglyoxime is also commonly added to achieve certain physical properties such as flow-ability. Further tailoring of physical properties is achieved by formulating unique concentrations of each constituent.
In dentistry, a veneer is a layer of material placed over a tooth. Veneers can improve the aesthetics and function of a smile and protect the tooth's surface from damage.

A temporary crown is a temporary (short-term) crown used in dentistry. Like other interim restorations, it serves until a final (definitive) restoration can be inserted. Usually the temporary crown is constructed from acrylic resins (monomethacrylate-based/polymethacrylate-based) or, chemical-cure/light cure composite (dimethacrylate-based), although alternative systems using aluminium crown forms are occasionally used. Temporary crowns function to protect the tooth, prevent teeth shifting, provide cosmetics, shape the gum tissue properly, and prevent sensitivity.

A glass ionomer cement (GIC) is a dental restorative material used in dentistry as a filling material and luting cement, including for orthodontic bracket attachment. Glass-ionomer cements are based on the reaction of silicate glass-powder and polyacrylic acid, an ionomer. Occasionally water is used instead of an acid, altering the properties of the material and its uses. This reaction produces a powdered cement of glass particles surrounded by matrix of fluoride elements and is known chemically as glass polyalkenoate. There are other forms of similar reactions which can take place, for example, when using an aqueous solution of acrylic/itaconic copolymer with tartaric acid, this results in a glass-ionomer in liquid form. An aqueous solution of maleic acid polymer or maleic/acrylic copolymer with tartaric acid can also be used to form a glass-ionomer in liquid form. Tartaric acid plays a significant part in controlling the setting characteristics of the material. Glass-ionomer based hybrids incorporate another dental material, for example resin-modified glass ionomer cements (RMGIC) and compomers.
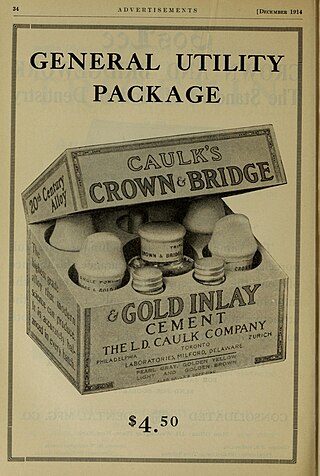
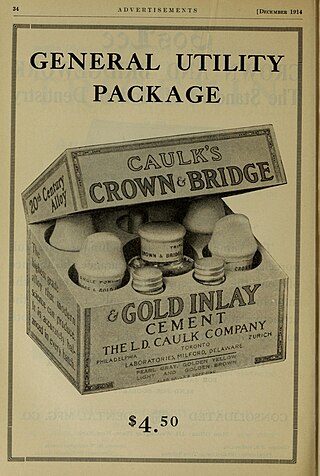
A luting agent is a dental cement connecting the underlying tooth structure to a fixed prosthesis. To lute means to glue two different structures together. There are two major purposes of luting agents in dentistry – to secure a cast restoration in fixed prosthodontics, and to keep orthodontic bands and appliances in situ.

CAD/CAM dentistry is a field of dentistry and prosthodontics using CAD/CAM to improve the design and creation of dental restorations, especially dental prostheses, including crowns, crown lays, veneers, inlays and onlays, fixed dental prostheses (bridges), dental implant supported restorations, dentures, and orthodontic appliances. CAD/CAM technology allows the delivery of a well-fitting, aesthetic, and a durable prostheses for the patient. CAD/CAM complements earlier technologies used for these purposes by any combination of increasing the speed of design and creation; increasing the convenience or simplicity of the design, creation, and insertion processes; and making possible restorations and appliances that otherwise would have been infeasible. Other goals include reducing unit cost and making affordable restorations and appliances that otherwise would have been prohibitively expensive. However, to date, chairside CAD/CAM often involves extra time on the part of the dentist, and the fee is often at least two times higher than for conventional restorative treatments using lab services.
Fixed prosthodontics is the branch of prosthodontics that focuses on dental prostheses that are permanently affixed (fixed). Crowns, bridges, inlays, onlays, and veneers are some examples of indirect dental restorations. Prosthodontists are dentists who have completed training in this specialty that has been recognized by academic institutes. Fixed prosthodontics can be used to reconstruct single or many teeth, spanning tooth loss areas. The main advantages of fixed prosthodontics over direct restorations are improved strength in big restorations and the possibility to build an aesthetic-looking tooth. The concepts utilised to select the suitable repair, as with any dental restoration, include consideration of the materials to be used, the level of tooth destruction, the orientation and placement of the tooth, and the condition of neighboring teeth
A post and core crown is a type of dental restoration required where there is an inadequate amount of sound tooth tissue remaining to retain a conventional crown. A post is cemented into a prepared root canal, which retains a core restoration, which retains the final crown.

In dentistry, amalgam is a liquid mercury and metal alloy mixture used to fill cavities caused by tooth decay.
A resin-retained bridge is a bridge replacing a missing tooth that relies for its retention on a composite resin cement. It is one of many available dental restoration methods which is considered minimally invasive and conservative of tooth tissue. The resin-retained-bridge has gone through a number of iterations. Perhaps the best known is the Maryland bridge and other designs used in the past include the Rochette bridge. The five-year survival rate is around 83.6% and the ten-year rate at 64.9%. The case selection is important and as with any dental prosthesis, good oral hygiene is paramount for success. In recent years, the indications for the use of resin-retained-bridges have diminished significantly and there have been changes in the principles underpinning their design. Resin-retained-bridges should be considered when a fixed prosthesis retained by natural teeth is required. The use has been driven by the advent of evidence-based dentistry showing the benefits to patients of reduced tooth preparation and the importance of an intact enamel structure for the long-term health of the teeth. The bridge is currently in favour in the United Kingdom for these reasons. Indeed, recent contemporary research shows resin retained bridges have better success rates than implants and are a cheaper alternative.
Dental cements have a wide range of dental and orthodontic applications. Common uses include temporary restoration of teeth, cavity linings to provide pulpal protection, sedation or insulation and cementing fixed prosthodontic appliances. Recent uses of dental cement also include two-photon calcium imaging of neuronal activity in brains of animal models in basic experimental neuroscience.
Dental compomers, also known as polyacid-modified resin composite, are used in dentistry as a filling material. They were introduced in the early 1990s as a hybrid of two other dental materials, dental composites and glass ionomer cement, in an effort to combine their desirable properties: aesthetics for dental composites and the fluoride releasing ability for glass ionomer cements.
An Endodontic crown or endocrown is a single prostheses fabricated from reinforced ceramics, indicated for endodontically treated molar teeth that have significant loss of coronal structure. Endocrowns are formed from a monoblock containing the coronal portion invaded in the apical projection that fills the pulp chamber space, and possibly the root canal entrances; they have the advantage of removing lower amounts of sound tissue compared to other techniques, and with much lower chair time needed. They are luted to the tooth structure by an adhesive material. The ceramic can be milled using computer-aided techniques or molded under pressure. Endocrowns can be an alternative to conventional crown restorations.
Anterior teeth are one of the most scrutinized teeth, the size and shape and color of the anterior upper teeth plays an important role in dental aesthetics and smile aesthetics. A few aesthetic anterior problems could be solved with composite restorations. For example, dental caries, tooth fracture, enamel defects and diastemas. Composite restoration can also improve aesthetic by changing shape, color, length and alignment of teeth.
Atraumatic restorative treatment (ART) is a method for cleaning out tooth decay from teeth using only hand instruments and placing a filling. It does not use rotary dental instruments to prepare the tooth and can be performed in settings with no access to dental equipment. No drilling or local anaesthetic injections are required. ART is considered a conservative approach, not only because it removes the decayed tissue with hand instruments, avoiding removing more tissue necessary which preserves as much tooth structure as possible, but also because it avoids pulp irritation and minimises patient discomfort. ART can be used for small, medium and deep cavities caused by dental caries.



![Gold Onlay [L] and Inlay [R] Dental inlays Gold Focus stacking with freeware CombineZP 12 02.jpg](http://upload.wikimedia.org/wikipedia/commons/thumb/2/22/Dental_inlays_Gold_Focus_stacking_with_freeware_CombineZP_12_02.jpg/191px-Dental_inlays_Gold_Focus_stacking_with_freeware_CombineZP_12_02.jpg)