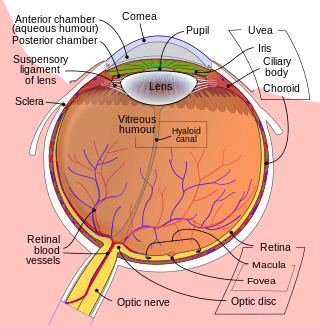
The retina is the innermost, light-sensitive layer of tissue of the eye of most vertebrates and some molluscs. The optics of the eye create a focused two-dimensional image of the visual world on the retina, which then processes that image within the retina and sends nerve impulses along the optic nerve to the visual cortex to create visual perception. The retina serves a function which is in many ways analogous to that of the film or image sensor in a camera.

Ophthalmology is a clinical and surgical specialty within medicine that deals with the diagnosis and treatment of eye disorders. A former term is oculism.

In neuroanatomy, the optic nerve, also known as the second cranial nerve, cranial nerve II, or simply CN II, is a paired cranial nerve that transmits visual information from the retina to the brain. In humans, the optic nerve is derived from optic stalks during the seventh week of development and is composed of retinal ganglion cell axons and glial cells; it extends from the optic disc to the optic chiasma and continues as the optic tract to the lateral geniculate nucleus, pretectal nuclei, and superior colliculus.
The National Eye Institute (NEI) is part of the U.S. National Institutes of Health (NIH), an agency of the U.S. Department of Health and Human Services. The mission of NEI is "to eliminate vision loss and improve quality of life through vision research." NEI consists of two major branches for research: an extramural branch that funds studies outside NIH and an intramural branch that funds research on the NIH campus in Bethesda, Maryland. Most of the NEI budget funds extramural research.
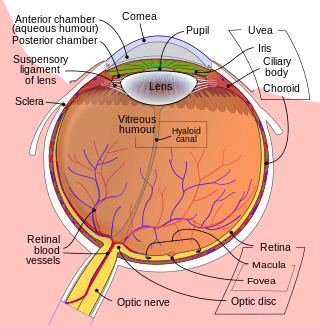
The aqueous humour is a transparent water-like fluid similar to blood plasma, but containing low protein concentrations. It is secreted from the ciliary body, a structure supporting the lens of the eyeball. It fills both the anterior and the posterior chambers of the eye, and is not to be confused with the vitreous humour, which is located in the space between the lens and the retina, also known as the posterior cavity or vitreous chamber. Blood cannot normally enter the eyeball.

A retinal ganglion cell (RGC) is a type of neuron located near the inner surface of the retina of the eye. It receives visual information from photoreceptors via two intermediate neuron types: bipolar cells and retina amacrine cells. Retina amacrine cells, particularly narrow field cells, are important for creating functional subunits within the ganglion cell layer and making it so that ganglion cells can observe a small dot moving a small distance. Retinal ganglion cells collectively transmit image-forming and non-image forming visual information from the retina in the form of action potential to several regions in the thalamus, hypothalamus, and mesencephalon, or midbrain.

Retinal detachment is a disorder of the eye in which the retina peels away from its underlying layer of support tissue. Initial detachment may be localized, but without rapid treatment the entire retina may detach, leading to vision loss and blindness. It is a surgical emergency.

The ciliary body is a part of the eye that includes the ciliary muscle, which controls the shape of the lens, and the ciliary epithelium, which produces the aqueous humor. The aqueous humor is produced in the non-pigmented portion of the ciliary body. The ciliary body is part of the uvea, the layer of tissue that delivers oxygen and nutrients to the eye tissues. The ciliary body joins the ora serrata of the choroid to the root of the iris.

The optic disc or optic nerve head is the point of exit for ganglion cell axons leaving the eye. Because there are no rods or cones overlying the optic disc, it corresponds to a small blind spot in each eye.
Vision science is the scientific study of visual perception. Researchers in vision science can be called vision scientists, especially if their research spans some of the science's many disciplines.

Müller glia, or Müller cells, are a type of retinal glial cells, first recognized and described by Heinrich Müller. They are found in the vertebrate retina, where they serve as support cells for the neurons, as all glial cells do. They are the most common type of glial cell found in the retina. While their cell bodies are located in the inner nuclear layer of the retina, they span across the entire retina.

Epiretinal membrane or macular pucker is a disease of the eye in response to changes in the vitreous humor or more rarely, diabetes. Sometimes, as a result of immune system response to protect the retina, cells converge in the macular area as the vitreous ages and pulls away in posterior vitreous detachment (PVD).
Köllner's Rule is a term used in ophthalmology and optometry that pertains to the progressive nature of color vision loss that is secondary to eye disease. This rule states that outer retinal diseases and media changes result in blue-yellow color defects, while diseases of the inner retina, optic nerve, visual pathway, and visual cortex will result in red-green defects. This is possibly related to the increased susceptibility of S-cones and rods to ischaemia and oxidative damage, although S-cone loss is more noticeable due to their lower density and their higher metabolic rate.
Proliferative vitreoretinopathy (PVR) is a disease that develops as a complication of rhegmatogenous retinal detachment. PVR occurs in about 8–10% of patients undergoing primary retinal detachment surgery and prevents the successful surgical repair of rhegmatogenous retinal detachment. PVR can be treated with surgery to reattach the detached retina but the visual outcome of the surgery is very poor. A number of studies have explored various possible adjunctive agents for the prevention and treatment of PVR, such as methotrexate, although none have yet been licensed for clinical use.
Sohan Singh Hayreh was an ophthalmologist, clinical scientist, and professor emeritus of ophthalmology at the University of Iowa. As one of the pioneers in the field of fluorescein angiography, he was generally acknowledged to be a leading authority in vascular diseases of the eye and the optic nerve. For over 60 years, Hayreh was actively involved in basic, experimental, and clinical research in ophthalmology, publishing over 400 original peer-reviewed articles in various international ophthalmic journals, six classical monographs and books in his field of research, and more than 50 chapters in ophthalmic books. He made many seminal observations dealing with the ocular circulation in health and disease, the optic disc and the optic nerve, retinal and choroidal vascular disorders, glaucomatous optic neuropathy, fundus changes in malignant arterial hypertension, ocular neovascularization, rheumatologic disorders of the eye, and nocturnal arterial hypotension. He was an elected fellow of the National Academy of Medical Sciences.
Retinal gene therapy holds a promise in treating different forms of non-inherited and inherited blindness.

King-Wai Yau is a Chinese-born American neuroscientist and Professor of Neuroscience at Johns Hopkins University School of Medicine in Baltimore, Maryland.
Joel S. Schuman, MD, FACS is Professor of Ophthalmology, the Kenneth L. Roper Endowed Chair, Vice Chair for Research Innovation, co-director of the Glaucoma Service at Wills Eye Hospital, Professor of Biomedical Engineering at Drexel University School of Biomedical Engineering, Science and Health Systems, Collaborative Community of Ophthalmic Imaging (CCOI) president, and American Glaucoma Society (AGS) Foundation advisory board chair. Prior to this he was the Elaine Langone Professor and Vice Chair for Research in the Department of Ophthalmology at NYU Langone Medical Center, NYU Grossman School of Medicine; Professor of Biomedical Engineering and Electrical & Computer Engineering at NYU Tandon School of Engineering and Professor of Neural Science in the Center for Neural Science at NYU College of Arts and Sciences. He chaired the ophthalmology department at NYU Langone Health, NYU Grossman School of Medicine 2016–2020, and was Vice Chair for Ophthalmology Research in the department 2020–2022. Prior to arriving at NYU in 2016, he was Distinguished Professor and Chairman of Ophthalmology, Eye and Ear Foundation Endowed Chair in Ophthalmology, Director of UPMC Eye Center (2003-2016) and before that was at Tufts University 1991–2003, where he was Residency Director (1991-1999) and Glaucoma and Cataract Service Chief (1991-2003). In 1998 he became Professor of Ophthalmology, and Vice Chair in 2001.

Robert E. MacLaren FMedSci FRCOphth FRCS FACS VR is a British ophthalmologist who has led pioneering work in the treatment of blindness caused by diseases of the retina. He is Professor of Ophthalmology at the University of Oxford and Honorary Professor of Ophthalmology at the UCL Institute of Ophthalmology. He is a Consultant Ophthalmologist at the Oxford Eye Hospital. He is also an Honorary Consultant Vitreo-retinal Surgeon at the Moorfields Eye Hospital. MacLaren is an NIHR Senior Investigator, or lead researcher, for the speciality of Ophthalmology. In addition, he is a member of the research committee of Euretina: the European Society of Retina specialists, Fellow of Merton College, in Oxford and a Fellow of the Higher Education Academy.
Michael Belkin is an Israeli academic and researcher working in ophthalmology, Professor Emeritus of Ophthalmology at Tel Aviv University. His research brought about advances in glaucoma treatment such as the ExPress glaucoma implant, the Ioptimate CO2 laser glaucoma surgery and a fast, non-contact glaucoma laser treatment.